What is cholesterol?
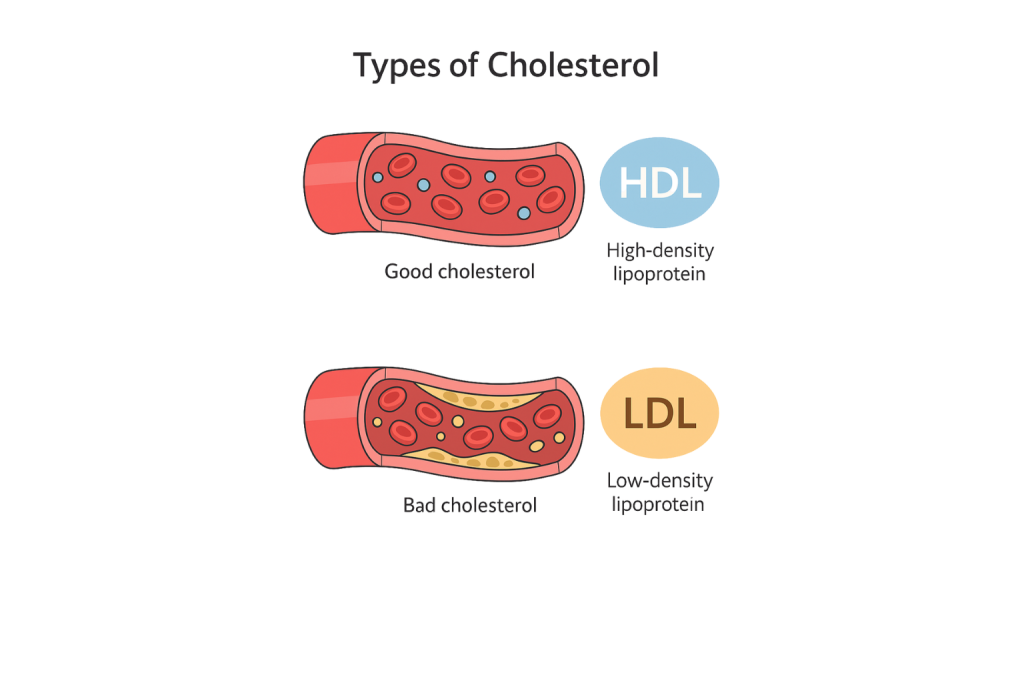
Seonat / September 12, 2025 / Cardiology What is cholesterol? Simple Definition: Cholesterol is a type of fat that is found in your blood. It is made by the liver and also comes from the food you eat. FAQ regarding this disease Can I feel if I have high cholesterol? No, high cholesterol does not cause symptoms. The only way to know is with a blood test. Does eating eggs raise cholesterol? Eggs contain cholesterol, but for most people they do not raise blood cholesterol much. Saturated and trans fats in processed foods are more likely to increase cholesterol levels. Do I need medicine if my cholesterol is high? Not always. Sometimes lifestyle changes are enough. Your doctor will decide if medicine is needed based on your cholesterol level and other risk factors. Expanded definition on Cholesterol Cholesterol is a type of fat that is found in your blood. It is made by the liver and also comes from the food you eat. Your body needs cholesterol to build cells, make hormones, and help with digestion. However, too much cholesterol in the blood can increase the risk of heart disease and stroke. Cholesterol itself is not bad. Problems happen when levels get out of balance. If there is too much of the harmful type, it can build up in the arteries and make them narrower, stopping blood from flowing properly. Are there different types of cholesterol? Yes. There are two main types that doctors talk about. Low-density lipoprotein (LDL) is often called “bad cholesterol”. This is because it can stick to the walls of arteries and form fatty deposits known as plaque. Over time, this makes the arteries hard and narrow, a process called atherosclerosis. High-density lipoprotein (HDL) is known as “good cholesterol”. It helps carry cholesterol away from the arteries and back to the liver, where it can be broken down and removed. Higher levels of HDL can protect against heart disease. Doctors also measure triglycerides, which are another type of fat in the blood. High triglyceride levels combined with high LDL and low HDL can raise the risk of health problems even more. Why does high cholesterol matter? High cholesterol itself does not cause symptoms, so many people do not know they have it. But over time, fatty deposits (plaque) can build up in the arteries, making them stiffer and narrower. This increases the risk of serious conditions such as coronary artery disease, heart attack, and stroke. The danger is that cholesterol can silently damage the arteries for years before any problems appear. That is why testing and prevention are so important. What causes high cholesterol? The only way to know your cholesterol level is with a blood test. This can be a finger-prick test in a clinic or a sample taken from your arm. The test measures total cholesterol, LDL, HDL, and triglycerides. In the UK, adults are usually advised to have their cholesterol checked every five years, or more often if they have risk factors such as high blood pressure, diabetes, or a family history of heart disease. What is a healthy cholesterol level? Doctors usually look at the balance between LDL and HDL rather than just the total number. A healthy total cholesterol level is generally considered to be 5 mmol/L or less. LDL should ideally be 3 mmol/L or less, while HDL should be 1 mmol/L or above. Targets may be stricter for people who already have heart disease, diabetes, or other risks. Can cholesterol be lowered? Yes, in many cases cholesterol can be lowered through lifestyle changes. Eating less saturated fat, such as fatty meat, butter, and processed foods, helps. Choosing more fruit, vegetables, wholegrains, and oily fish is beneficial. Regular exercise can raise good cholesterol and lower bad cholesterol. Losing weight, cutting down on alcohol, and stopping smoking also make a big difference. If lifestyle changes are not enough, medicines called statins may be prescribed. Statins reduce the amount of cholesterol made by the liver and are proven to lower the risk of heart attacks and strokes. Other medicines such as ezetimibe or newer injectable drugs may also be used. Who is most at risk of high cholesterol? Anyone can have high cholesterol, but some groups are more at risk. People with unhealthy diets, those who are overweight, or who do little exercise are more likely to develop it. Family history, increasing age, and certain medical conditions also raise the risk. Men tend to have higher cholesterol earlier in life, while women’s risk rises after menopause. Prevalence of high cholesterol in adults in the UK This chart shows that around 40% of UK adults have high cholesterol, which is more than 17 million people. The remaining 60% have levels within the recommended range. High cholesterol is a major risk factor for heart and circulatory diseases. Can high cholesterol be prevented? In many cases, yes. A balanced diet, regular exercise, and not smoking are the most effective steps. Keeping to a healthy weight and having regular cholesterol checks also help. Even small changes, like walking more, eating less processed food, and drinking less alcohol, can lower cholesterol levels. What happens if high cholesterol is not treated? Untreated high cholesterol increases the risk of fatty deposits building up in the arteries. This can lead to angina, heart attacks, strokes, and peripheral arterial disease. The longer cholesterol stays high, the more damage it can do. That is why early testing and treatment are important. What is life like with high cholesterol? For many people, managing high cholesterol simply means adopting healthier habits. Medicines may also be needed, especially if other risk factors are present. With treatment, most people can reduce their risk and live full, active lives. Monitoring is ongoing. Regular check-ups with a GP, staying on top of medicines, and keeping a healthy lifestyle all form part of long-term care. Conclusion Coronary artery disease happens when the arteries supplying the heart become narrowed or blocked by fatty deposits. It often causes angina and
What is coronary artery disease?
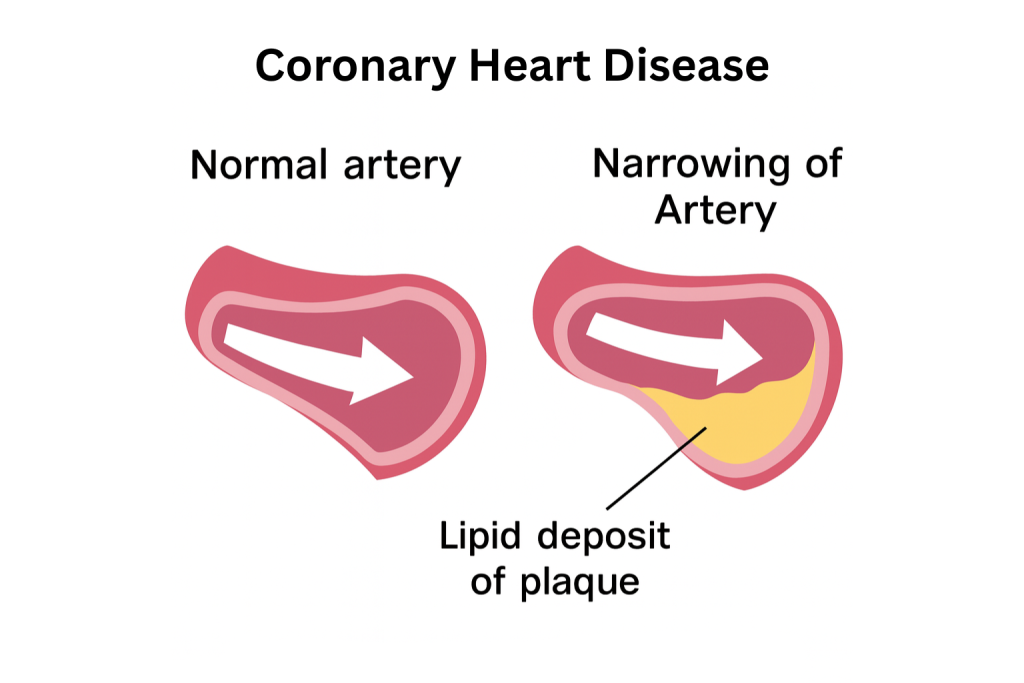
Seonat / September 11, 2025 / Cardiology What is coronary artery disease? Simple Definition: Coronary artery disease is when the blood vessels that supply the heart, called the coronary arteries, become narrowed or blocked. FAQ regarding this disease Can I exercise if I have coronary artery disease? Yes, gentle and regular exercise is often encouraged, but it should be guided by your doctor. Cardiac rehabilitation programmes can help you exercise safely. Does coronary artery disease always cause symptoms? No, some people have no symptoms until the disease is advanced or they have a heart attack. Regular check-ups are important if you have risk factors. Is coronary artery disease the same as angina? No, angina is a symptom of coronary artery disease. The disease itself is the narrowing of the arteries, while angina is the chest pain that results from reduced blood flow. Expanded definition on CAD Coronary artery disease is when the blood vessels that supply the heart, called the coronary arteries, become narrowed or blocked. This happens because fatty deposits, also known as plaque, build up inside the artery walls. Over time, this reduces the flow of oxygen-rich blood to the heart muscle. It is one of the most common types of heart disease and a leading cause of illness and death worldwide. In the UK, thousands of people are affected, but the condition is often preventable and treatable with the right care. How does coronary artery disease develop? The condition develops gradually over many years through a process called atherosclerosis. At first, fatty deposits may not cause any problems. But as they grow, the arteries become narrower and stiffer. This limits how much blood can reach the heart. Sometimes, the plaque can rupture, leading to a blood clot forming inside the artery. If the clot blocks blood flow completely, it can cause a heart attack. What does coronary artery disease feel like? The most common symptom is angina, which is chest pain or discomfort caused by reduced blood flow to the heart. Angina often feels like pressure, heaviness, or tightness in the chest, and it can spread to the arms, neck, jaw, or back. It is usually triggered by physical activity or emotional stress and eases with rest. Other symptoms can include breathlessness, fatigue, or palpitations. Sometimes, people have no symptoms until the disease becomes advanced or until they have a heart attack. What causes coronary artery disease? Most of the time, no. That is why it is dangerous. Many people have high blood pressure for years without knowing. In very severe cases, symptoms like headaches, blurred vision, chest pain, or nosebleeds can happen, but these are rare and often linked to extremely high readings. Because symptoms are uncommon, the only reliable way to know if you have high blood pressure is to get it measured. Is coronary artery disease the same as heart disease? Coronary artery disease is the most common type of heart disease, but the term “heart disease” can include other conditions too. For example, problems with heart valves, abnormal rhythms, or heart muscle disease are all types of heart disease. Coronary artery disease specifically refers to blockages in the arteries that supply the heart. How is coronary artery disease diagnosed? Doctors usually start with a discussion of symptoms and risk factors. They may check blood pressure, cholesterol levels, and blood sugar. An electrocardiogram (ECG) can show if there are problems with the heart’s rhythm or past damage. Other tests include echocardiograms, CT scans, or MRI scans to look at the heart’s structure and function. A coronary angiogram may be done, where dye is injected into the arteries to see blockages on an X-ray. These tests help confirm the diagnosis and guide treatment. How is it treated? Treatment usually combines lifestyle changes, medicines, and sometimes medical procedures. Lifestyle changes include eating a healthier diet, being more active, quitting smoking, and reducing alcohol. These steps not only help manage the disease but also prevent it from getting worse. Medicines often prescribed include statins to lower cholesterol, beta-blockers to reduce strain on the heart, and aspirin or other drugs to prevent clots. When arteries are very narrow, procedures may be needed. Angioplasty with a stent can widen the artery and improve blood flow. In more severe cases, coronary artery bypass surgery may be performed, where new routes are created for blood to reach the heart. Risk factors for people in the UK This chart shows the main risk factors for coronary artery disease in UK adults. Around 1 in 4 adults have high blood pressure, while 4 in 10 have high cholesterol. Smoking remains a major contributor, with about 13% of adults still smoking. These factors significantly increase the chances of developing coronary artery disease. Can coronary artery disease be cured? There is no cure that completely removes the disease, but it can be controlled. Treatments can relieve symptoms, improve quality of life, and reduce the risk of heart attacks. Many people live long and active lives after diagnosis if they follow their treatment plan carefully. Is it dangerous? Yes, untreated coronary artery disease can be life-threatening. It increases the risk of heart attacks, heart failure, and abnormal heart rhythms. However, with treatment and lifestyle changes, the risks can be greatly reduced. The earlier it is diagnosed, the easier it is to manage. Can it be prevented? Prevention is one of the most important aspects of coronary artery disease. Stopping smoking, eating a balanced diet, exercising regularly, and maintaining a healthy weight all help protect the arteries. Keeping blood pressure, cholesterol, and diabetes under control also lowers the risk. Regular health checks are important, especially for people with a family history of heart disease. Prevention is not always possible, but healthy habits make a big difference. What is life like with coronary artery disease? Living with the condition often means making changes. Medicines may be needed long term, and follow-up appointments are important. But with the right care, many people continue to work, exercise, and enjoy
What is High Blood Pressure?
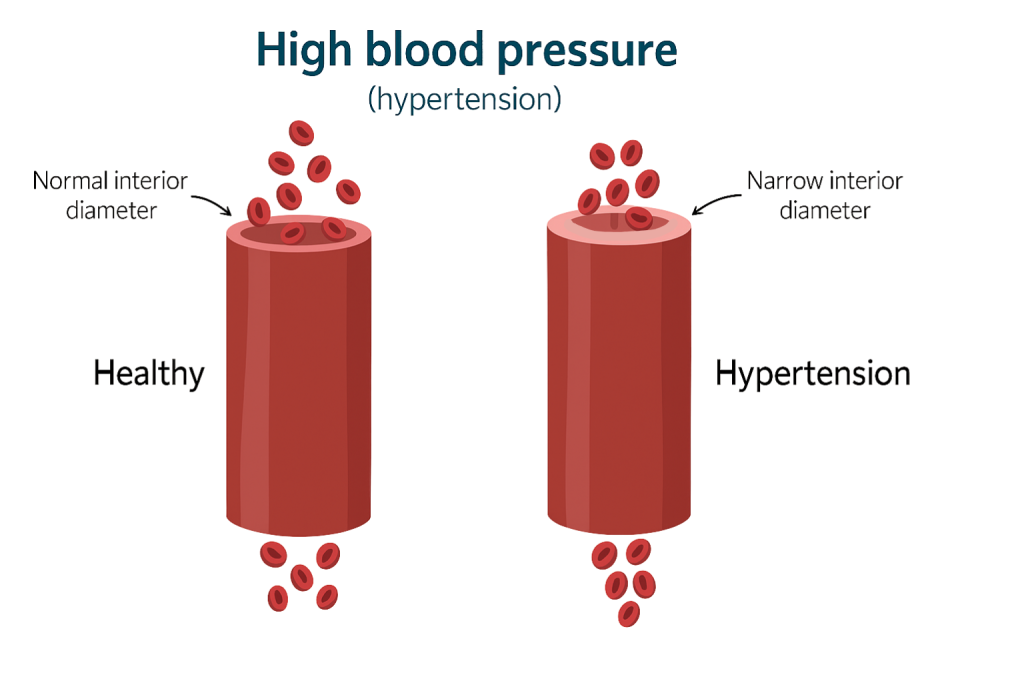
Seonat / September 10, 2025 / Cardiology What is High Blood Pressure? Simple Definition: High blood pressure, also called hypertension, is when the force of blood pushing against the walls of your arteries is consistently too high. FAQ if you are after quick questions and answers Can stress cause high blood pressure? Stress can raise blood pressure for short periods, and long-term stress may contribute to unhealthy habits like poor diet or smoking, which increase the risk of high blood pressure. Can high blood pressure go away on its own? High blood pressure usually does not go away without treatment. Lifestyle changes and, if needed, medicines are the best way to control it. Is high blood pressure the same as hypertension? Yes, hypertension is just the medical term for high blood pressure. Expanded definition High blood pressure, also called hypertension, is when the force of blood pushing against the walls of your arteries is consistently too high. Arteries are the blood vessels that carry blood from the heart to the rest of the body. When the pressure is too strong for too long, it can damage the arteries and increase the risk of heart disease, stroke, kidney problems, and other serious conditions. Blood pressure is measured in millimetres of mercury (mmHg) and written as two numbers. The first number, called systolic pressure, is the pressure when the heart contracts and pumps blood. The second number, called diastolic pressure, is the pressure when the heart relaxes between beats. A normal reading is usually around 120/80 mmHg. High blood pressure is generally diagnosed when readings are consistently 140/90 mmHg or above. Why does high blood pressure matter? High blood pressure is often called the “silent killer” because it does not usually cause obvious symptoms, but over time it quietly damages the body. It makes the heart work harder, which can cause the heart muscle to thicken and weaken. It also damages artery walls, making them stiffer and more likely to get blocked. This is why high blood pressure is one of the biggest risk factors for strokes, heart attacks, and heart failure. This chart shows the different categories of blood pressure, measured in millimetres of mercury (mmHg). It compares systolic pressure (the top number, when the heart contracts) and diastolic pressure (the bottom number, when the heart relaxes). Green represents normal blood pressure, yellow shows elevated levels, and the shades of orange and red highlight increasing stages of high blood pressure. The darker the colour, the greater the health risk, with a hypertensive crisis needing urgent medical attention. What causes high blood pressure? There is not always a single cause. For many people, it develops gradually with age. Factors that increase the chances include being overweight, eating too much salt, drinking too much alcohol, smoking, and not getting enough exercise. Stress can also play a role. Other medical conditions, such as diabetes, kidney disease, and thyroid problems, can also lead to high blood pressure. In some cases, medicines like steroids or contraceptive pills may contribute. Does high blood pressure have symptoms? Most of the time, no. That is why it is dangerous. Many people have high blood pressure for years without knowing. In very severe cases, symptoms like headaches, blurred vision, chest pain, or nosebleeds can happen, but these are rare and often linked to extremely high readings. Because symptoms are uncommon, the only reliable way to know if you have high blood pressure is to get it measured. How is high blood pressure diagnosed? Doctors usually check blood pressure with a cuff that goes around the upper arm. The test is quick and painless. Because pressure can change during the day, a diagnosis is not made from a single reading. Instead, doctors often take several measurements over time, or ask patients to wear a monitor for 24 hours to get an average result. If you want to visit a private clinic, places like Heartsure offer the 24 hour holder monitor. If readings are consistently high, the diagnosis is confirmed. Doctors may also check blood and urine to look for related problems, and sometimes order scans or heart tests to see if any damage has been caused. Who is most at risk of high blood pressure? Anyone can develop it, but it is more common as people get older. Family history plays a role too. People of African or Caribbean descent are at higher risk. Lifestyle is also important—those who smoke, are overweight, or eat a diet high in salt are more likely to have it. Men are slightly more likely than women to develop high blood pressure before age 55, but after this age, women are just as likely to be affected. Can high blood pressure be treated? Yes, it can. For many people, lifestyle changes are enough to lower blood pressure. Losing weight, exercising regularly, eating less salt, and cutting down on alcohol all help. Stopping smoking and managing stress are also important. When lifestyle changes alone are not enough, medicines are often prescribed. These include diuretics, ACE inhibitors, calcium channel blockers, and beta-blockers. The choice depends on age, other health conditions, and side effects. Many people take more than one medicine to keep blood pressure under control. What happens if high blood pressure is not treated? If left untreated, high blood pressure can cause serious long-term problems. It increases the risk of heart attack, stroke, kidney disease, heart failure, and vascular dementia. Damage builds up slowly over the years, which is why early diagnosis and treatment are so important. Can high blood pressure be prevented? In many cases, yes. Prevention is very similar to treatment. Keeping to a healthy weight, exercising regularly, eating plenty of fruit and vegetables, and limiting salt and alcohol all help keep blood pressure at safe levels. Regular check-ups are important, especially for people with a family history or other risk factors. Even small changes, such as walking more, cutting down on processed foods, or reducing stress, can make a big difference. What is
What is a pacemaker?
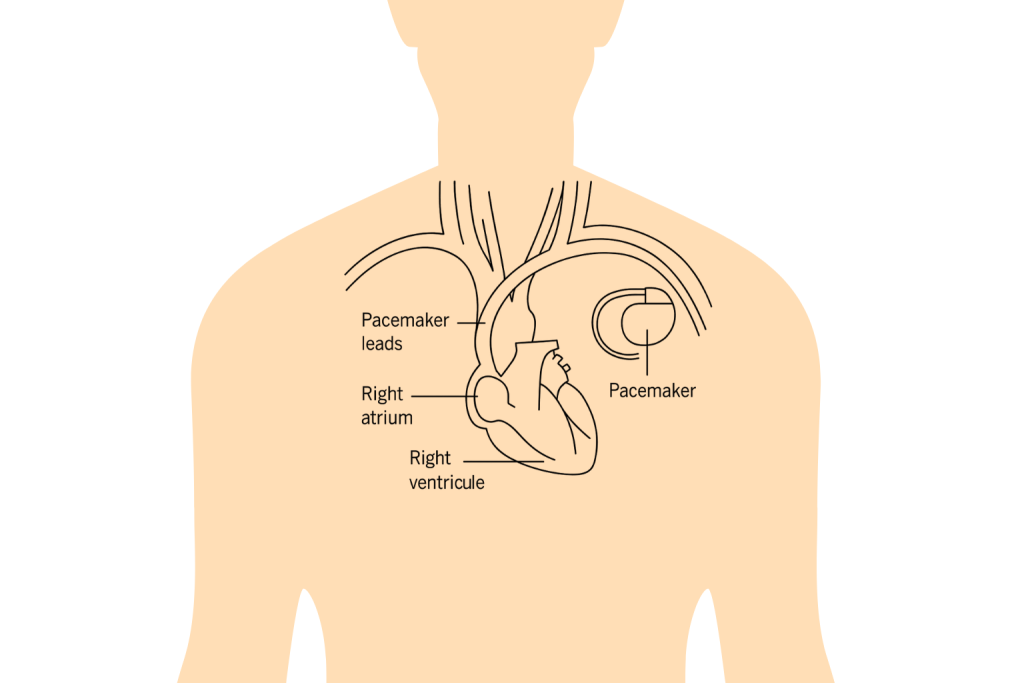
Seonat / September 9, 2025 / Cardiology What is a pacemaker? A pacemaker is a small medical device that helps control the heartbeat. FAQ if you are after quick answers Can I use a mobile phone with a pacemaker? Yes, mobile phones are safe to use, but it is best to keep them at least six inches away from the pacemaker. Using the opposite ear to the side of your implant is usually advised. Will I need another pacemaker later in life? Pacemaker batteries last between 5 and 15 years. When the battery runs low, the device can be replaced with a simple procedure, so many people do have more than one pacemaker in their lifetime. Can I exercise if I have a pacemaker? Most people can return to normal activities and exercise after recovery. Strenuous movements should be avoided for the first few weeks, but long term, exercise is encouraged to keep the heart healthy. Are pacemakers safe around airport security machines? Yes, pacemakers are safe with airport scanners. However, carrying your pacemaker ID card is helpful, as staff may offer a manual check instead. Can I live a normal life with a pacemaker? Yes, most people live full, active lives with a pacemaker. It helps control symptoms and improve quality of life, though some precautions and regular check-ups are needed. Why would someone need a pacemaker? The heart has its own natural electrical system that tells it when to beat. If this system is damaged or does not work properly, the heart rhythm may become irregular. This is known as arrhythmia. Some arrhythmias are harmless, but others can cause serious symptoms. A pacemaker is used when medicines alone are not enough to keep the heart rhythm stable. People who faint, feel weak, or experience sudden drops in heart rate may be advised to have one fitted. How does a pacemaker work? A pacemaker is made up of two main parts: a small battery-powered generator and thin wires called leads. The generator sits under the skin of the chest, while the leads are guided into the heart. The pacemaker watches the heart’s rhythm and, when needed, sends tiny pulses of electricity to keep it steady. These pulses are so small that you do not feel them. The device can be programmed by doctors to match each patient’s needs. Some pacemakers are temporary, used for a short period, while others are permanent. How is a pacemaker fitted? The procedure is usually done under local anaesthetic, meaning you are awake but the area is numbed. A small cut is made under the collarbone, and the leads are guided into the heart using X-ray images. The generator is then placed under the skin and connected to the leads. The whole procedure usually takes about one to two hours. Most people stay in hospital overnight and go home the next day. Recovery is fairly quick, although heavy lifting and strenuous exercise should be avoided for a few weeks. Does it hurt to have a pacemaker? Fitting a pacemaker is not painful because of the anaesthetic. Afterwards, there may be some bruising or soreness in the chest, which usually improves within days. Most people say they get used to the feeling of having a device under the skin quite quickly. What is life like with a pacemaker? Life with a pacemaker is often much better than before, as it helps control symptoms caused by irregular heart rhythms. Most people can return to normal activities, including work, exercise, and travel. Certain precautions are advised. Strong magnets or powerful electrical equipment can interfere with the pacemaker, so patients are usually given advice on what to avoid. Airport security machines, for example, are safe, but carrying a pacemaker card helps explain why you may need a manual check. Modern pacemakers can be checked remotely, allowing doctors to monitor how they are working without frequent hospital visits. The batteries last between 5 and 15 years, depending on the type, and can be replaced with a simple procedure. Are pacemakers safe? Yes, pacemakers are very safe and widely used. Complications are rare, but as with any procedure, there are small risks. These include infection at the implant site, bleeding, or movement of the leads. Doctors carefully check patients before fitting a pacemaker to make sure it is the right choice. Once fitted, regular follow-ups help keep everything working properly. Can you feel a pacemaker working? Most people cannot feel their pacemaker working. The electrical pulses are so small that they are not noticeable. Occasionally, someone may feel a brief flutter in the chest if the pacemaker corrects an irregular rhythm, but this is usually harmless. Do pacemakers cure heart disease? A pacemaker does not cure the underlying cause of heart disease. Instead, it helps manage the symptoms of irregular rhythms by keeping the heartbeat steady. Medicines and lifestyle changes may still be needed alongside a pacemaker to protect long-term heart health. Who usually needs a pacemaker? Pacemakers are often used in people with slow heart rhythms, such as those caused by heart block. They can also be used in people with heart failure, where the heart struggles to pump effectively, or in those with other rhythm problems like atrial fibrillation. Age is a factor too. As people get older, the heart’s electrical system can naturally wear out, making pacemakers more common in older adults. However, younger people can also need them if they have certain heart conditions. Round up A pacemaker is a small device that helps control irregular heart rhythms by sending electrical signals to the heart. It is fitted under the skin with thin wires that connect to the heart muscle. The procedure is safe, quick, and widely used to treat arrhythmias that cause symptoms like fainting, dizziness, and breathlessness. While a pacemaker does not cure heart disease, it can greatly improve quality of life and reduce risks linked to abnormal rhythms. With regular check-ups and a few lifestyle precautions, most people with pacemakers live long
What is Cardiac Arrest?
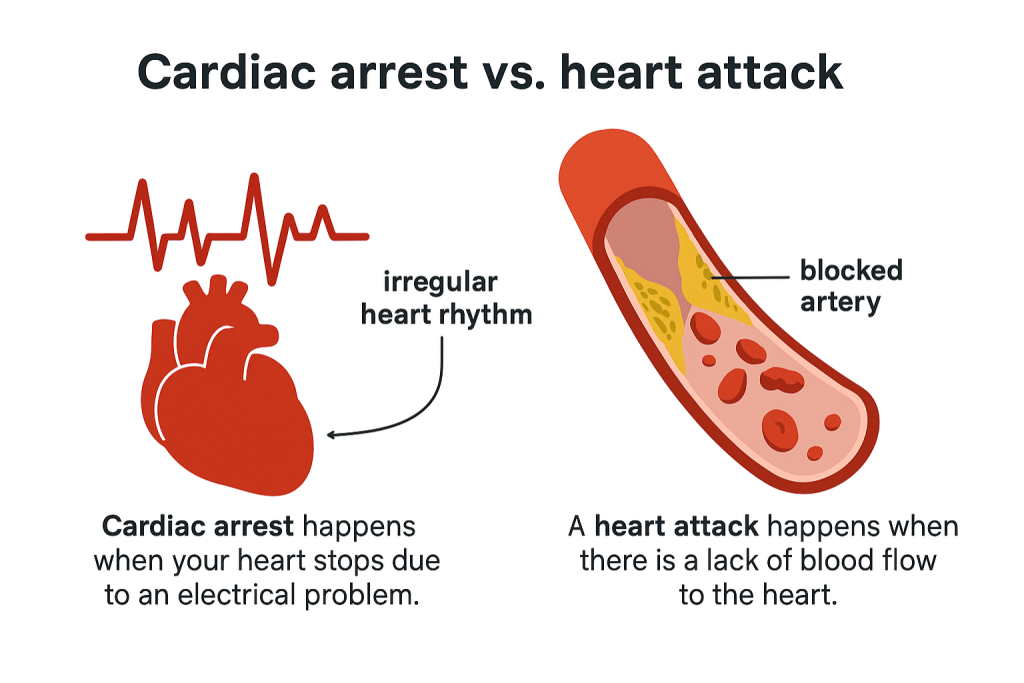
Seonat / September 8, 2025 / Uncategorized What is Cardiac Arrest? Cardiac arrest is when the heart suddenly stops pumping blood around the body. It is a life-threatening emergency and different from a heart attack, even though the two are often confused. When the heart stops, blood and oxygen can no longer reach the brain and other vital organs. Without immediate treatment, cardiac arrest can cause death within minutes. How does cardiac arrest happen? The heart beats because of electrical signals that control how the muscles contract. In cardiac arrest, these signals go wrong, leading to an irregular rhythm called an arrhythmia. The most common arrhythmia linked to cardiac arrest is ventricular fibrillation, where the lower chambers of the heart quiver instead of pumping properly. This electrical problem means the heart cannot pump blood effectively. In some cases, the heart may stop beating altogether. Is cardiac arrest the same as a heart attack? No, they are different conditions. A heart attack happens when blood flow to part of the heart muscle is blocked, often by a clot or plaque build up. The heart usually keeps beating during a heart attack, although it is under strain. Cardiac arrest, on the other hand, means the heart stops working suddenly. Sometimes a heart attack can trigger a cardiac arrest, but they are not the same. Knowing the difference is important, because both need urgent treatment but in different ways. What does cardiac arrest look like? Someone having a cardiac arrest will usually collapse suddenly. They will lose consciousness and will not be breathing normally, or may stop breathing altogether. They will have no pulse. Unlike a faint, the person does not wake up within a minute or two. Without immediate help, they will not survive. This is why recognising cardiac arrest quickly and starting emergency care is so important. What should you do if someone has a cardiac arrest? If someone collapses and is not breathing, the first step is to call 999 immediately. Paramedics can provide advanced care, but while waiting, cardiopulmonary resuscitation (CPR) should be started straight away. CPR involves pressing hard and fast in the centre of the chest to keep blood flowing to the brain and organs. If a defibrillator is available, it should be used as soon as possible. Defibrillators give an electric shock to reset the heart’s rhythm and can greatly increase survival chances. What causes cardiac arrest? There are several possible causes. The most common is coronary heart disease, where narrowed arteries reduce blood supply to the heart. A heart attack caused by this disease can sometimes trigger cardiac arrest. Other causes include heart rhythm disorders such as ventricular tachycardia or atrial fibrillation, heart failure, and inherited conditions that affect the electrical system of the heart. Cardiac arrest can also be caused by severe blood loss, choking, drowning, electrocution, or trauma. Sometimes it happens with no clear warning or known cause. Who is most at risk of cardiac arrest? People with heart disease are at the highest risk, especially those who have already had a heart attack or live with heart failure. Family history also matters, as inherited heart rhythm disorders can increase risk. Age plays a role, with older adults more likely to experience cardiac arrest, but it can happen to younger people too, particularly athletes with undiagnosed heart conditions. Lifestyle factors such as smoking, obesity, and lack of exercise also contribute to higher risk. Can cardiac arrest be prevented? Not all cases can be prevented, but many risk factors can be reduced. Looking after heart health by keeping blood pressure, cholesterol, and blood sugar under control lowers the risk. Stopping smoking, eating a balanced diet, staying active, and limiting alcohol all protect the heart. For people with known heart rhythm problems, doctors may recommend implantable cardioverter defibrillators (ICDs). These small devices are placed under the skin and can deliver a shock automatically if dangerous rhythms are detected, preventing cardiac arrest. How is cardiac arrest treated in hospital? Surviving cardiac arrest is life-changing. Some people recover quickly, while others may experience memory problems, tiredness, or emotional difficulties. Rehabilitation and follow-up care are important for both physical and mental recovery. Lifestyle changes become especially important after a cardiac arrest. Following medical advice, taking prescribed medicines, and attending regular check-ups all reduce the chances of future heart problems. Support from family, friends, and healthcare teams also plays a key role in long-term recovery. Is survival from cardiac arrest possible? Yes, survival is possible, but it depends heavily on how quickly treatment is given. Every minute without CPR or defibrillation reduces the chances of survival by about 10%. This is why knowing basic first aid and how to use a defibrillator can save lives. In the UK, public access defibrillators are now widely available in places like train stations, schools, and shopping centres. When used quickly, they can more than double the chances of surviving a cardiac arrest. Final Summary Cardiac arrest is when the heart suddenly stops pumping blood, causing loss of consciousness and breathing. It is a medical emergency that is different from a heart attack, although the two are linked. The main signs are sudden collapse, no breathing, and no pulse. Immediate action—calling 999, starting CPR, and using a defibrillator if available—is vital to save lives. While not all cases can be prevented, reducing risk factors such as smoking, high blood pressure, and poor diet can protect heart health. For survivors, follow-up care and lifestyle changes are key to recovery. Disclaimer: Seonat provides general health information for educational purposes only. This content is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your GP or another qualified health provider with any questions about a medical condition or before making health decisions.
What is Heart Failure?
Seonat / September 5, 2025 / Cardiology What is Heart Failure? Heart failure is a condition where the heart is not able to pump blood around the body as well as it should. Despite the name, it does not mean the heart has stopped working. Instead, it means the heart is weaker or stiffer than normal, so blood does not flow as effectively. This can cause tiredness, breathlessness, and fluid build-up in the body. Heart failure is common, especially in older adults, and it can develop gradually over time. With the right treatment and lifestyle changes, many people with heart failure can live active lives for many years. What causes heart failure? Heart failure is usually the result of other conditions that have damaged or weakened the heart. The most common causes include coronary heart disease, where the arteries supplying the heart become narrowed, and heart attacks, which can damage heart muscle. Other causes include high blood pressure, which makes the heart work harder, and conditions that affect the heart valves or rhythm. Sometimes heart failure is linked to infections, thyroid problems, or genetic conditions. In some cases, doctors cannot find a single cause. What does heart failure feel like? The symptoms of heart failure can vary, but the most common ones are breathlessness, tiredness, and swelling in the ankles, legs, or stomach. Some people find it hard to breathe when lying flat or wake up at night short of breath. Others may feel more tired than usual, even when doing simple activities. As the condition progresses, symptoms may become more noticeable and affect everyday life. How is heart failure diagnosed? Doctors use a combination of symptoms, examination, and tests to diagnose heart failure. A GP may listen to the chest, check for fluid build-up, and ask about medical history. Blood tests can show if the heart is under strain, while an electrocardiogram (ECG) can record the heart’s electrical activity. Imaging tests such as echocardiograms, chest X-rays, , or MRI scans can give detailed pictures of the heart’s structure and function. These tests help doctors confirm the diagnosis and decide on the best treatment. Are there different types of heart failure? Yes, heart failure can affect different parts of the heart. Left-sided heart failure happens when the left side of the heart is not pumping strongly enough. Right-sided heart failure means the right side is struggling, often because the left side is already weak. Doctors may also describe heart failure based on whether the heart muscle is too weak to squeeze properly or too stiff to relax and fill with blood. These types are called reduced ejection fraction and preserved ejection fraction. Is heart failure the same as a heart attack? No, they are different. A heart attack happens suddenly when a blood clot blocks an artery to the heart. This causes damage to the heart muscle. Heart failure, on the other hand, is usually a long-term condition that develops over time, often as a result of heart attacks, high blood pressure, or other heart problems. However, a heart attack can lead to heart failure if the damage is severe enough. How is heart failure treated? Although heart failure cannot usually be cured, it can be managed effectively. Treatment often involves medicines to help the heart work better, reduce symptoms, and prevent the condition from getting worse. Common medicines include ACE inhibitors, beta-blockers, diuretics, and mineralocorticoid receptor antagonists. In some cases, devices such as pacemakers or defibrillators are fitted to help control the heartbeat. Severe cases may require surgery, such as valve repair or, in rare cases, a heart transplant. Lifestyle changes are also very important. Eating a healthy diet, reducing salt intake, staying active, avoiding smoking, and limiting alcohol can all improve heart health. What happens if heart failure is not treated? Without treatment, heart failure usually gets worse over time. Symptoms such as breathlessness and fatigue can become more severe, and the risk of hospital admissions increases. Untreated heart failure can also shorten life expectancy. This is why it is important to seek medical advice if you notice symptoms, as treatment can greatly improve both quality of life and survival. Who is most at risk of heart failure? Heart failure is more common in older people, but anyone can develop it. Risk increases if you have had a heart attack, have high blood pressure, or live with conditions like diabetes, obesity, or long-term kidney disease. Family history also plays a role, and men are slightly more likely than women to develop it. Lifestyle factors such as smoking, lack of exercise, and a poor diet can also increase the risk. Can heart failure be prevented? Not all cases can be prevented, but many risk factors can be managed. Keeping blood pressure and cholesterol under control, eating well, exercising regularly, and not smoking are key steps. Regular health checks can also spot problems early, reducing the chance of developing heart failure later on. If you already have heart disease, following your treatment plan carefully can lower your risk of developing heart failure. What is life like with heart failure? Life with heart failure can be challenging, but with treatment and support many people manage it well. Symptoms may limit what you can do, but cardiac rehabilitation programmes, lifestyle advice, and medicines all help. Emotional health is also important, as living with a long-term condition can cause stress or anxiety. Support from family, friends, and healthcare teams makes a big difference. Many people find that once they understand their condition and know how to manage symptoms, they feel more in control and able to live a fulfilling life. Summary Heart failure is a condition where the heart does not pump blood as effectively as it should. It is usually caused by other heart problems such as coronary heart disease, heart attacks, or high blood pressure. The main symptoms are breathlessness, tiredness, and swelling in the body. Although it cannot usually be cured, heart failure can be managed with medicines, lifestyle
What is a Stent?
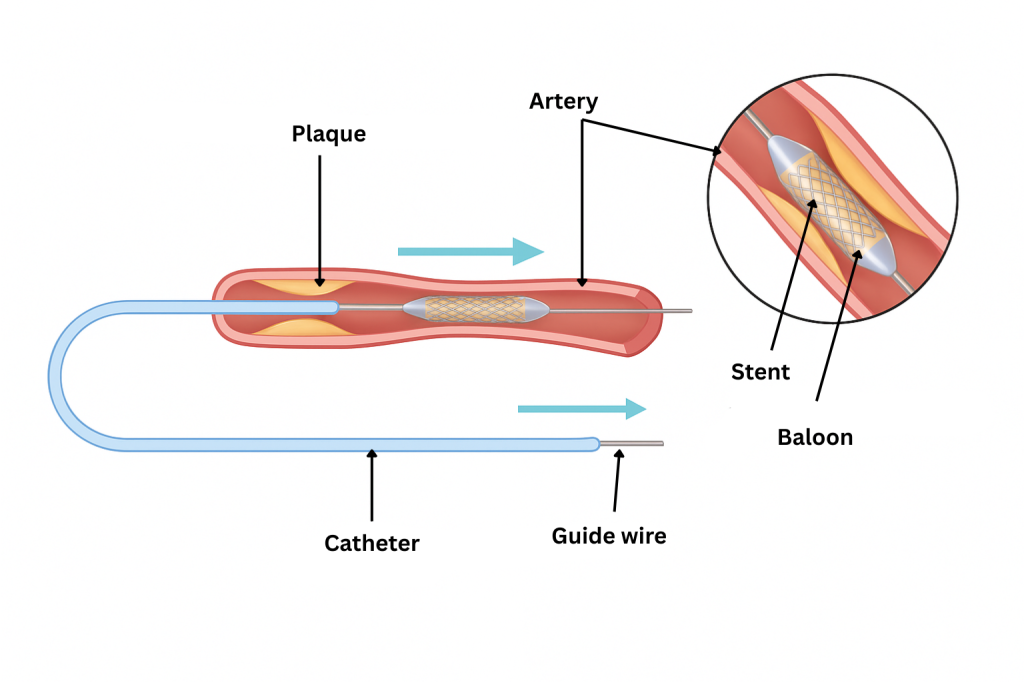
Seonat / September 4, 2025 / Cardiology What is a Stent? A stent is a small tube made of metal or plastic that is placed inside an artery or another passage in the body to help keep it open. In heart care, stents are most often used in the coronary arteries, which supply blood to the heart. If these arteries become narrowed or blocked by fatty deposits, blood flow to the heart can be reduced, leading to chest pain or even a heart attack. By placing a stent inside the artery, doctors can restore normal blood flow. The stent acts like a scaffold, holding the artery open and reducing the chance of it closing again. Why are stents used? Stents are used to treat narrowed or blocked arteries caused by coronary heart disease. Over time, fatty deposits known as plaque can build up inside the artery walls, making them hard and narrow. This process is called atherosclerosis. When this happens in the coronary arteries, the heart muscle does not get enough oxygen-rich blood, causing symptoms such as angina. If left untreated, the blockage can lead to a heart attack. Stents are a common and effective way of opening up arteries to restore blood supply and reduce the risk of serious problems. How is a stent put in? The procedure is called angioplasty with stent placement. It is usually carried out in a hospital’s catheterisation laboratory by a cardiologist. A thin tube called a catheter is inserted into an artery, often through the wrist or groin, and guided to the heart. At the tip of the catheter is a tiny balloon with the stent around it. When the balloon is inflated, it pushes the plaque against the artery wall and expands the stent. The balloon is then deflated and removed, leaving the stent in place to hold the artery open. The procedure normally takes between 30 minutes and 2 hours, depending on how many arteries are treated. Does having a stent hurt? The procedure is not painful because local anaesthetic is used at the catheter site, and patients are usually given medicine to help them relax. Some people feel a bit of pressure in the chest when the balloon is inflated, but this only lasts a few seconds. After the procedure, there may be mild soreness or bruising where the catheter was inserted, but this usually improves quickly. What are stents made of? Most stents are made of a special metal mesh, often stainless steel or cobalt-chromium. These are designed to be strong but flexible enough to fit inside an artery. Some stents are bare metal, while others are coated with a medicine that slowly releases into the artery wall. These are called drug-eluting stents and help reduce the risk of the artery becoming narrow again. How long do stents last? Once in place, stents are designed to be permanent. The artery wall usually grows around the stent, making it part of the blood vessel. However, in some cases, the artery can become narrow again inside the stent. This is known as restenosis. Drug-eluting stents reduce the chances of this happening compared to bare-metal stents. Is having a stent safe? Stent procedures are very common and generally safe, but like all medical treatments, they carry some risks. Possible complications include bleeding at the catheter site, damage to the artery, or an allergic reaction to the dye used in the procedure. Rarely, the artery can close up again or a blood clot can form inside the stent. To reduce risks, patients are usually prescribed medicines such as aspirin and other blood thinners for several months after the procedure. These help stop clots from forming inside the stent. What happens after having a stent? After the procedure, patients are taken to a recovery area for monitoring. Most people stay in hospital overnight and go home the next day. They are advised to avoid heavy lifting or strenuous activity for about a week. Follow-up appointments with a cardiologist are important to check progress. Patients are usually advised to keep taking prescribed medicines, eat a heart-healthy diet, exercise regularly, and stop smoking if they do. These steps help protect the stent and reduce the risk of further heart problems. How does life change with a stent? Many people feel a big improvement in symptoms such as chest pain or breathlessness soon after the procedure. Quality of life often improves because blood flow to the heart is restored. Most people return to normal activities within a week or two. Long-term, having a stent is a reminder that lifestyle changes are important. Stents treat the blockage, but they do not cure the underlying heart disease. Eating well, exercising, and taking medicines as advised are all crucial for long-term heart health. Are there alternatives to a stent? Yes, depending on the severity and location of the blockage. Medicines such as nitrates, beta-blockers, or statins can sometimes control symptoms without surgery. Another option is coronary artery bypass surgery, where new routes are created for blood to flow around blockages. This is usually recommended when there are multiple or severe blockages that cannot be treated with stents alone. In some cases, newer treatments such as rotablation may be used before stenting to prepare the artery if the blockage is very hard or calcified. Should I get a stent on the NHS or privately? In the UK, stents are widely available on the NHS for people who need them. They are commonly used in emergencies, such as during a heart attack, as well as for planned procedures to treat angina. Private treatment may be faster and offer more flexibility in choosing a hospital, but the procedure itself is essentially the same. Can you feel a stent inside your body? No, you cannot feel the stent once it is in place. It becomes part of the artery wall and does not cause any sensation. Some people worry about having a piece of metal in their body, but stents are designed to
What is Rotablation?
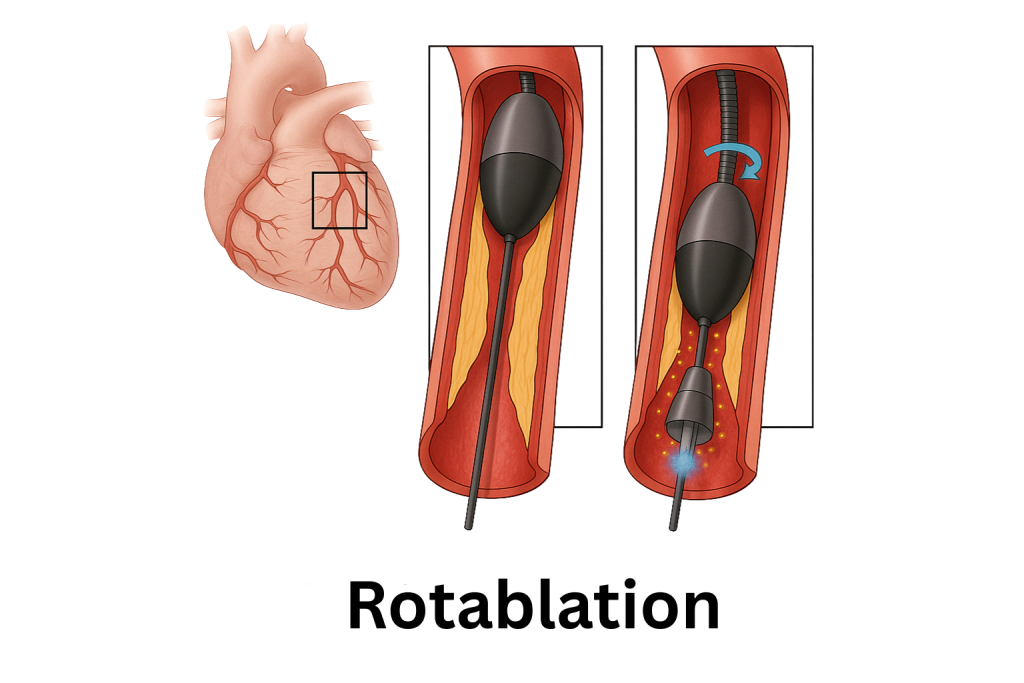
Seonat / September 3, 2025 / Cardiology What is Rotablation? Rotablation is a medical procedure used to treat very hard or heavily calcified blockages in the heart’s arteries. These blockages stop blood flowing properly and can lead to chest pain, breathlessness, or heart attacks. Rotablation helps by using a tiny drill with a diamond-coated tip to grind away the hard calcium inside the artery. This makes it easier for doctors to widen the artery with a stent and restore normal blood flow to the heart. It is usually done when standard treatments like balloon angioplasty do not work because the artery is too stiff or blocked with calcium. Why would someone need rotablation? Rotablation is often used in people with severe coronary artery disease where the artery walls have become hardened with calcium. As we age, or if we have risk factors like high cholesterol, diabetes, or high blood pressure, fatty deposits and calcium can build up in the arteries. In some cases, the calcium becomes so solid that balloons and stents cannot get through. This is where rotablation is useful, as it clears a path so that other treatments can be carried out successfully. Without it, some people might not be able to have life-saving procedures to restore blood flow. How does rotablation work? The procedure is carried out in a cardiac catheterisation laboratory by a specialist team. A thin tube called a catheter is inserted, usually through an artery in the wrist or groin, and guided to the heart. At the end of this catheter is the tiny drill, which spins at very high speed. The tip of the drill is covered with microscopic diamond particles, which gently grind away the calcium in the artery. The tiny fragments are broken down into dust-like particles, which are washed away harmlessly in the bloodstream. Once enough calcium is removed, the artery can be widened with a balloon and a stent can be placed to keep it open. Does rotablation hurt? The procedure itself is not painful, because local anaesthetic is used where the catheter is inserted. Patients are usually awake but given medicine to help them relax. Some people may feel pressure in the chest during the procedure, but pain is uncommon. Afterward, there may be mild bruising or soreness at the insertion site, but this usually improves within a few days. How long does rotablation take? The procedure usually takes between 30 minutes and 2 hours, depending on how many arteries are being treated and how complex the blockages are. Most patients stay in hospital overnight for monitoring, but some may go home the same day if everything is straightforward. Is rotablation safe? Rotablation is generally considered safe, but like all medical procedures it carries some risks. Possible complications include damage to the artery, irregular heart rhythms, or the artery closing up again. Serious complications are rare, especially when the procedure is performed by experienced cardiologists. For many patients, the benefits of rotablation outweigh the risks, as it allows successful treatment in cases where other methods would fail. Who carries out rotablation? The procedure is performed by an interventional cardiologist, a doctor who specialises in treating heart disease with minimally invasive techniques. They work with a team of nurses, radiographers, and technicians in the catheterisation lab. The team monitors the patient closely throughout the procedure, keeping track of heart rhythm, blood pressure, and oxygen levels. What happens after rotablation? After the procedure, patients are taken to a recovery area where they are monitored for a few hours. Most people are advised to lie flat for a short time if the catheter was inserted through the groin. If it was done through the wrist, recovery is often quicker. Patients usually go home within one or two days and are advised to avoid heavy lifting or strenuous exercise for about a week. Medicines such as blood thinners are often prescribed to prevent clots from forming around the stent. Follow-up appointments with a cardiologist are arranged to check progress and ensure the artery is healing well. What are the benefits of rotablation? The main benefit is that it makes it possible to treat heavily calcified blockages that would otherwise be very difficult or impossible to fix. By clearing a pathway through the calcium, rotablation allows stents to be placed securely. This improves blood flow to the heart, relieves chest pain, and reduces the risk of heart attack. For many patients, this means a better quality of life, with fewer symptoms and more energy for everyday activities. Are there alternatives to rotablation? In some cases, other treatments may be considered. Standard balloon angioplasty and stenting are often used first, but they may not work if the artery is too hard. In rare cases, bypass surgery may be an alternative, but this is a more invasive operation. Another newer technique called orbital atherectomy works in a similar way to rotablation, using a different type of spinning device to remove calcium. However, rotablation remains one of the most widely used and proven methods. Can rotablation cure heart disease? Rotablation does not cure the underlying cause of heart disease. It clears blockages to improve blood flow, but the build-up of fatty deposits and calcium can continue if risk factors are not controlled. This is why lifestyle changes and medicines remain important after the procedure. Eating a healthy diet, exercising regularly, stopping smoking, and taking prescribed medicines such as statins or blood pressure tablets all help protect the arteries from further damage. What is life like after rotablation? Most people feel an improvement in symptoms such as chest pain or shortness of breath soon after the procedure. Recovery is usually quicker than with open-heart surgery, and many patients return to normal activities within a week or two. Long-term outcomes depend on overall health and lifestyle choices. With proper care, many people go on to live active and fulfilling lives after rotablation. Regular check-ups with a cardiologist are important to monitor heart health and prevent further problems.
What is an ECG Test?

Seonat / September 1, 2025 / Cardiology What is an ECG Test? An ECG test, also called an electrocardiogram, is a simple and painless way for doctors to check how your heart is working. It records the electrical activity of the heart and shows whether it is beating normally. The test is quick, safe, and widely used in hospitals, clinics, and GP surgeries. ECG tests are important because they help doctors spot heart problems early. They can show if your heartbeat is irregular, if the heart is under strain, or if there has been damage such as a heart attack. How does the heart’s electricity work? The heart beats because of tiny electrical signals that travel through it. These signals make the heart muscles contract and pump blood around the body. If the signals are too fast, too slow, or disrupted, the heartbeat may not be regular. An ECG test records these signals and draws them as a graph with waves and spikes. Each part of the graph shows a stage of the heartbeat cycle, giving doctors clues about how well the heart is working. The heart’s electrical system starts in the sinoatrial (SA) node, which is the natural pacemaker. The signal then moves to the atrioventricular (AV) node, where it pauses slightly to let the atria contract. From there, it travels down the Bundle of His, which splits into the right and left bundle branches. Finally, the impulse spreads through the Purkinje fibres, making the ventricles contract and pump blood. How does an ECG test work? During the test, small sticky pads called electrodes are placed on your skin. These are usually put on the chest, arms, and legs. The pads are connected by wires to the ECG machine, which records the heart’s electrical activity. You will be asked to lie still while the machine records for a few seconds or minutes. The results are shown on a screen or printed out for a doctor to read. The test does not hurt, and the only thing you may feel is the coolness of the pads when they are placed on your skin. When is an ECG test needed? Doctors recommend an ECG test when someone has symptoms that could be linked to the heart. This includes chest pain, palpitations, dizziness, fainting, or shortness of breath. It can also be done if you already have heart disease, to monitor your condition, or if you are taking medicines that may affect the heart. Some people have an ECG before surgery to check that their heart is healthy enough for anaesthetic. Are there different types of ECG test? Yes, there are a few types depending on what the doctor needs to find out. The most common is a resting ECG, which is done while lying still. This shows how the heart works at rest. Another type is an exercise ECG, also called a stress test. This is done while walking on a treadmill or cycling on an exercise bike. It helps doctors see how the heart responds to physical activity. There is also a Holter monitor, which is a small device you wear for 24 hours or longer. It records the heart’s activity over a full day, picking up irregularities that may not appear during a short test. What does an ECG show? An ECG test can give a lot of useful information. It can show if your heart is beating too quickly or too slowly, or if the rhythm is irregular. It can also show signs of a previous heart attack, problems with blood flow to the heart, or changes caused by conditions such as high blood pressure. Sometimes an ECG shows small changes that suggest the heart is not getting enough oxygen. This can be a warning sign of angina or blocked arteries. How long does an ECG test take? A resting ECG usually takes about 5 to 10 minutes, including the time to attach the electrodes. The recording itself only takes a few seconds. Exercise ECGs and Holter monitoring take longer, but even then, the process is simple and non-invasive. Do I need to prepare for an ECG test? There is very little preparation needed. You may be asked to remove jewellery or clothing from the upper body so that electrodes can be placed on the skin. Sometimes men may need a small area of chest hair shaved to help the pads stick properly. Otherwise, you can eat, drink, and take your medicines as normal unless told otherwise by your doctor. What happens after the test? After a resting ECG, the electrodes are removed, and you can go straight home or back to your normal activities. The results may be available immediately, or they may need to be reviewed by a cardiologist. If anything unusual is found, your doctor may suggest further tests, such as blood tests, an echocardiogram, or a heart scan. Can an ECG test diagnose all heart problems? No, an ECG cannot detect every heart issue. Some problems only happen from time to time, which is why longer monitoring may be needed. For example, an irregular heartbeat might not appear during a short test but could be caught with a Holter monitor. Other heart conditions, such as minor valve problems, may not show up on an ECG and may need other scans or tests. An ECG is usually the first step in finding out what is wrong, but it may need to be combined with other investigations. What do abnormal ECG results mean? An abnormal result does not always mean something is seriously wrong. Sometimes changes are due to harmless variations in heart rhythm, or even technical factors such as how the electrodes were placed. Doctors always look at ECG results alongside symptoms and medical history to decide what they mean. If the ECG does show a problem, it might point to conditions such as atrial fibrillation, angina, or evidence of a past heart attack. It may also reveal if the heart is enlarged or
What is Angina?

Seonat / August 29, 2025 / Cardiology What is Angina? Angina is chest pain or discomfort that happens when your heart doesn’t get enough blood and oxygen, usually because the arteries are narrowed. Angina is a common condition that affects the heart, but many people are unsure what it actually means. Some think it is the same as a heart attack, while others confuse it with general chest pain. Understanding angina is important because it can be a warning sign of underlying heart disease. Knowing what it is, why it happens, and what to do about it can help people recognise symptoms early and get the right treatment. So, what is angina? It is not a disease on its own but a symptom of coronary heart disease, the most common type of heart condition in the UK. When the arteries that supply blood to the heart become narrowed or blocked, less blood reaches the heart muscle. This causes pain or discomfort, often triggered by physical activity or emotional stress, when the heart has to work harder. Angina does not always feel the same for everyone. Some people describe it as a heaviness or pressure, while others say it feels like squeezing, burning, or tightness in the chest. What does angina feel like? The classic symptom of angina is chest discomfort, but the way it feels can vary. Many people feel pressure or a heavy weight in the middle of the chest. The pain can also spread to the shoulders, arms, neck, jaw, or back. Some people may feel short of breath, sick, sweaty, or unusually tired at the same time. For some, angina symptoms are mild and last only a few minutes. For others, the pain is stronger and more frequent. Women and people with diabetes sometimes experience angina in less typical ways, such as stomach pain, indigestion-like discomfort, or tiredness rather than clear chest pain. Are there different types of angina? Yes, doctors describe angina in several forms. The most common is stable angina. This happens in a predictable pattern, usually triggered by exercise or stress, and it often improves with rest or medication. Unstable angina is more serious. It can occur suddenly, at rest, or with very little effort, and the pain tends to last longer. This is a warning sign that a heart attack may be about to happen, and it requires urgent medical attention. Another type, called variant angina or Prinzmetal’s angina, is less common. It is caused by temporary spasms in the coronary arteries, which reduce blood flow. This type can happen even when resting and may come and go in cycles. What causes angina? The main cause is coronary heart disease. This happens when fatty deposits build up inside the arteries, a process known as atherosclerosis. The arteries become narrow and stiff, making it harder for blood to flow freely. Certain factors increase the chances of developing angina. These include smoking, high blood pressure, high cholesterol, diabetes, being overweight, and lack of exercise. Age and family history also play a role. Men over 45 and women over 55 are more likely to develop it, especially if heart disease runs in the family. How is angina different from a heart attack? Although the symptoms can feel similar, angina is not the same as a heart attack. In angina, the reduced blood flow to the heart is temporary. The discomfort usually goes away after a few minutes of rest or medicine. A heart attack, on the other hand, happens when blood flow is completely blocked, usually by a blood clot. The pain is more severe, lasts longer, and does not go away with rest. A heart attack causes permanent damage to the heart muscle if not treated quickly. Because the symptoms can overlap, anyone who experiences sudden or severe chest pain should call 999 immediately, as it may be a heart attack rather than angina. How is angina diagnosed? Doctors use several methods to diagnose angina. A GP will usually start by asking about symptoms, medical history, and lifestyle. Blood pressure and cholesterol checks are often done, along with blood tests to look for signs of heart disease. Further tests may include an electrocardiogram (ECG) to record the heart’s electrical signals, an echocardiogram to see how the heart is pumping, or a stress test to check how the heart performs during exercise. In some cases, CT scans, MRI scans, or coronary angiograms are used to look directly at the heart and its arteries. What treatments are available? Treatment for angina aims to reduce symptoms, improve quality of life, and lower the risk of heart attack or stroke. Lifestyle changes are often the first step. Stopping smoking, eating a balanced diet, exercising regularly, and managing stress all help reduce strain on the heart. Medicines are also commonly prescribed. Nitrates, such as glyceryl trinitrate (GTN) spray, relax and widen blood vessels, quickly easing pain. Other medicines, including beta-blockers, calcium channel blockers, statins, and aspirin, may be given to lower blood pressure, reduce cholesterol, or prevent clots. For more severe angina, procedures may be needed. Angioplasty with a stent can open narrowed arteries, while bypass surgery creates new routes for blood to flow around blockages. Can angina be cured? There is no permanent cure for angina, because it is a sign of underlying heart disease. However, with treatment and lifestyle changes, symptoms can be managed very effectively. Many people live long, active lives with angina once it is under control. Is angina dangerous? Angina itself does not usually cause permanent damage, but it is a warning sign of serious heart disease. It means that the heart is struggling to get enough blood, which increases the risk of a heart attack or stroke. Unstable angina is particularly dangerous and should always be treated as a medical emergency. Who is more likely to get angina? Angina is more common in people with certain risk factors. These include: Age over 45 for men and 55 for women Smoking High blood pressure
