When Should I Get My Heart Checked?

Seonat / August 28, 2025 / Cardiology When Should I Get My Heart Checked? The heart is one of the most important organs in the body, pumping blood and oxygen to keep everything working. Heart disease remains a leading cause of illness and death in the UK, knowing when to get your heart checked can make a big difference. Many problems can be treated more effectively if they are found early. A heart check can spot risk factors, detect hidden issues, and give you peace of mind about your health. What does a heart check involve? A heart check can include several different tests, depending on your age, medical history, and symptoms. The most basic checks are blood pressure and cholesterol tests, which help assess the risk of heart disease. Blood sugar tests can also be used to look for diabetes, which is closely linked to heart problems. Other tests include electrocardiograms (ECG) to measure the heart’s electrical activity, echocardiograms to see how the heart muscle and valves are working, and scans such as CT or MRI for a more detailed look. A GP may also ask about lifestyle habits, family history, and symptoms such as chest pain or breathlessness. Should I get my heart checked if I feel healthy? Yes, sometimes it is still a good idea. Heart disease can develop silently without obvious symptoms. Risk factors like high blood pressure and high cholesterol often go unnoticed for years. Having a routine check, especially if you are over 40, can help pick up issues early. Even if you feel healthy, checks can provide reassurance and encourage good habits. At what age should I start thinking about a heart check? In the UK, people between 40 and 74 are eligible for an NHS Health Check every five years. This looks at blood pressure, cholesterol, weight, and lifestyle, giving an overall picture of heart health. Younger adults may also benefit from checks if they have risk factors such as diabetes, obesity, or a strong family history of heart disease. Children and young people usually do not need routine heart checks unless there are symptoms or known conditions. However, if there is a family history of sudden heart problems at a young age, doctors may recommend screening earlier. What symptoms mean I should see a doctor sooner? Some symptoms should never be ignored. Chest pain, pressure, or discomfort—especially if it happens during exercise—can be a sign of coronary heart disease. Shortness of breath, palpitations, fainting, or swelling in the legs may also point to problems. If you develop sudden or severe chest pain, you should call 999 immediately, as this could be a heart attack. Even mild or occasional symptoms are worth discussing with a GP, as they may suggest further tests. Early treatment often means better outcomes. How often should I get my heart checked? The frequency depends on your age and risk factors. Most healthy adults only need checks as part of their routine NHS Health Check every five years from age 40. People with high blood pressure, diabetes, high cholesterol, or a family history of heart disease may need more regular reviews. If you are on treatment for heart problems, your doctor will arrange follow-up checks to monitor your condition. These may happen once a year or more often, depending on your health. Does family history make a difference? Yes, family history is an important factor. If a close relative, such as a parent or sibling, developed heart disease at a young age, your own risk may be higher. In these cases, it is often advised to get checked earlier and more regularly. Doctors may also suggest specific tests based on your family’s medical history. Can lifestyle choices mean I need a heart check earlier? Definitely. Lifestyle has a big impact on heart health. Smoking, heavy drinking, poor diet, and lack of exercise all increase the risk of problems. Being overweight, having high stress levels, or living with conditions such as diabetes also raise the chances of developing heart disease. If these apply to you, your GP may recommend earlier or more frequent checks. Is it better to go private for a heart check? Both NHS and private options are available. NHS Health Checks are free for eligible age groups, but waiting times can vary for more detailed tests. Private heart checks are usually faster and may offer a wider range of tests, such as CT coronary angiograms or advanced blood tests. The choice often depends on your personal situation, budget, and how quickly you want results. What happens after a heart check? If results are normal, you may simply be advised to continue with healthy habits. If risk factors are found, lifestyle changes or medicines may be recommended. For example, statins can lower cholesterol, while blood pressure tablets reduce strain on the heart. If tests show more serious issues, you may be referred to a cardiologist for specialist care. Can regular checks really prevent heart disease? While checks cannot stop heart disease from developing, they can catch problems early and reduce the risks. For example, treating high blood pressure or high cholesterol in the early stages can prevent heart attacks and strokes later in life. Checks also give people the knowledge they need to make healthier choices, which has a big effect on long-term heart health. Round Up Getting your heart checked is an important step in protecting your health. Most adults should start routine checks from the age of 40, but earlier testing may be needed if there are symptoms, family history, or lifestyle risks. Heart checks can be simple, quick, and highly effective in spotting problems before they become serious. Even if you feel healthy, it is worth considering, as many heart conditions develop silently. Acting early can make all the difference for your future health. Disclaimer: Seonat provides general health information for educational purposes only. This content is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your
What is Local Anaesthetic?

Seonat / August 26, 2025 / General Health What is Local Anaesthetic Local anaesthetic is a type of medicine that numbs a small part of the body so that you do not feel pain during a procedure. Unlike general anaesthetic, which makes you unconscious, local anaesthetic allows you to stay awake and alert. It is commonly used for minor operations, dental work, and certain diagnostic tests. The medicine is usually given by injection, cream, or spray. Once it takes effect, you may still feel pressure or movement, but you should not feel pain. Because it only works on a specific area, recovery is usually quicker, and you can often go home the same day. Why is local anaesthetic used? It is used whenever doctors need to perform a procedure without causing pain, but where full unconsciousness is not necessary. For example, dentists often use local anaesthetic for fillings and tooth extractions. It is also used for stitching wounds, removing small lumps, performing biopsies, and carrying out certain eye or skin operations. Local anaesthetic is preferred when the procedure is quick, when the risks of general anaesthetic are too high, or when it is better for the patient to stay awake. How does it work? Local anaesthetic works by blocking the nerves in a small area from sending pain signals to the brain. When the medicine is injected or applied, it stops the sodium channels in the nerve endings from working. This means the nerves cannot pass pain messages, and the area becomes numb. The effect usually starts within minutes and can last from half an hour to several hours, depending on the type and dose used. Doctors can also add other medicines, such as adrenaline, to make the numbing effect last longer. Lidocaine (a local anaesthetic) blocks sodium channels in nerves, stopping pain signals from travelling to the brain and causing numbness in the treated area. What does it feel like to have it? When given as an injection, you may feel a small sting at first. Within a few minutes, the area should feel heavy, warm, or tingly. Soon after, it becomes completely numb. You might still notice pressure or movement during the procedure, but it should not be painful. If a cream or spray is used, it may feel cool when applied. The area gradually loses sensation, making minor procedures more comfortable. Is local anaesthetic safe? For most people, local anaesthetic is very safe. Because it only affects a small area of the body, the risks are lower than with general anaesthetic. Side effects are usually mild and short-lived. The most common are bruising or soreness at the injection site, tingling once the numbness wears off, or temporary weakness in nearby muscles. Serious side effects are rare. In very unusual cases, the medicine can enter the bloodstream and cause dizziness, blurred vision, or an irregular heartbeat. This is why local anaesthetic is always given by trained staff who know how to avoid and manage complications. Who gives local anaesthetic? Local anaesthetic can be given by a wide range of healthcare professionals. Dentists use it daily for routine treatments. Doctors, nurses, and surgeons also use it in hospitals and clinics for minor operations. In more complex cases, an anaesthetist may be involved to choose the best medicine and dose. How long does it take to wear off? The numbness usually lasts one to two hours for small doses, and longer for larger procedures. In dental work, the feeling in your lips and tongue may last for several hours afterwards. As the medicine wears off, you may feel tingling before full sensation returns. Doctors often advise patients to avoid eating or drinking hot food until the numbness has gone, to prevent accidental burns or bites. What happens before and after? Before having local anaesthetic, the doctor or nurse will explain what to expect. They may ask about allergies, medicines you are taking, and any past reactions to anaesthetic. You do not usually need to fast beforehand, and you can normally go home straight after the procedure. Afterwards, the area may feel numb for some time. Once the effect wears off, there might be mild soreness, but this can usually be managed with over-the-counter pain relief if needed. Most people return to normal activities quickly. Can everyone have local anaesthetic? Almost everyone can have local anaesthetic safely. It is especially useful for people who may not be suitable for general anaesthetic, such as those with heart or lung problems. However, doctors will take extra care if a patient has certain health conditions, is pregnant, or has had allergic reactions to anaesthetic in the past. What are the different types of local anaesthetic? There are a few ways local anaesthetic can be given. Topical anaesthetic comes as a cream, gel, or spray and is applied directly to the skin or mouth. Injectable anaesthetic is delivered with a needle into the tissue near the nerves. Nerve blocks are injections placed close to a specific nerve to numb a larger area, such as an arm or leg. Regional anaesthesia, such as spinal or epidural injections, is sometimes grouped with local anaesthetic but works on a wider area. These are commonly used during childbirth or surgery on the lower body. What are the advantages of local anaesthetic? Local anaesthetic has several benefits. It avoids the risks linked to general anaesthetic, allows patients to recover more quickly, and usually means fewer side effects. People can often eat, drink, and move around soon after the procedure. It is also less disruptive for short or simple treatments. Can you be awake during surgery with local anaesthetic? Yes. In fact, this is one of the main features of local anaesthetic. You remain awake and aware, but the area being treated is numb, so you should not feel pain. For more complicated procedures, sedation can sometimes be added. This makes you drowsy and relaxed, while still avoiding full unconsciousness. Are there alternatives to local anaesthetic? Yes. For very small
What is General Anaesthetic?

Seonat / August 25, 2025 / General Health What is General Anaesthetic? General anaesthetic is a type of medicine used during surgery to make a person completely unconscious and unable to feel pain. Unlike a local anaesthetic, which numbs only one part of the body, general anaesthetic affects the whole body. It ensures that patients do not feel, hear, or remember the procedure taking place. General anaesthesia is usually given by injection into a vein or by breathing in gases through a mask. It is carefully controlled by an anaesthetist, a doctor who specialises in this field. While under general anaesthetic, your vital signs such as heart rate, breathing, and blood pressure are monitored closely at all times. Why is general anaesthetic used? It is used when an operation would be too painful or complex for a local or regional anaesthetic. For example, procedures on the chest, abdomen, brain, or heart almost always require general anaesthesia. It is also chosen when patients need to remain very still for a long period or when muscle relaxation is essential for the surgery. Some people also require general anaesthetic if they are anxious or if the operation would otherwise be too distressing. How does it work? General anaesthetic works by interfering with the way nerves carry signals in the brain and body. Once the medicines enter the bloodstream, they act quickly to block pain signals and reduce awareness. Within seconds, the patient becomes unconscious. While the person is asleep, a breathing tube may be inserted into their windpipe to make sure they get enough oxygen. The level of anaesthetic is adjusted throughout the operation to keep the patient safely unconscious, and then it is gradually reduced when the surgery is complete. This diagram shows how anaesthetic medicines affect the brain. On the left, without anaesthetic, a small amount of chloride flows through the GABA receptor, which only slightly calms brain activity. On the right, with anaesthetic (such as propofol or sevoflurane), the medicine helps the receptor stay open longer, allowing more chloride to enter. This increased flow makes brain cells much quieter, which helps the body relax, fall asleep, and stay pain-free during surgery. What happens before it is given? Before surgery, patients usually meet the anaesthetist to talk through their medical history. They are asked about allergies, medicines, past reactions to anaesthetic, and whether they smoke or drink alcohol. These details help the anaesthetist decide which drugs and doses to use. Patients are also asked not to eat or drink for several hours before surgery. This is to reduce the risk of food or liquid entering the lungs while unconscious. Sometimes pre-medication is given to help people relax or reduce stomach acid before the operation. What does it feel like to go under? Most people describe the feeling as very quick. After the injection or breathing in the anaesthetic gas, there is usually a light-headed sensation followed by rapid drowsiness. Many patients report that it feels like going to sleep instantly, with no memory of the time that passes. Waking up can feel like only moments later, even if the operation has taken hours. What are the side effects? Most side effects are short-term and improve within a few hours or days. These include feeling sick, shivering, a sore throat from the breathing tube, and temporary confusion or drowsiness. Older people may take longer to recover and sometimes feel more confused for a day or two after surgery. Less common side effects include allergic reactions, chest infections, or awareness during surgery, though the latter is very rare thanks to modern monitoring. Serious complications, such as damage to the heart or brain, are extremely uncommon and usually linked to existing health conditions. Is general anaesthetic safe? For most people, general anaesthetic is very safe. Advances in medicine, better monitoring equipment, and highly trained anaesthetists mean that the risks are much lower than in the past. However, the level of risk depends on the patient’s overall health, age, and the type of surgery. People with conditions such as heart disease, diabetes, obesity, or breathing problems may face slightly higher risks. This is why the pre-operative assessment is important, as it allows the team to prepare and reduce any dangers. Who gives general anaesthetic? In the UK, general anaesthetic is given by an anaesthetist. This is a fully qualified doctor with specialist training in anaesthesia, pain relief, and critical care. They stay with the patient throughout the operation, adjusting the dose and watching vital signs to keep everything stable. A team of anaesthetic nurses and operating department practitioners usually assist. How long does it take to recover afterwards? After surgery, patients are taken to a recovery room where nurses monitor them closely until they are fully awake. Most people wake up within minutes, although grogginess can last for a few hours. Some feel sick, but anti-sickness medicines are often given to help. Recovery times vary depending on the type of surgery. For minor operations, patients may go home the same day. For major surgery, a hospital stay of several days or longer is common. It may take a few days to feel fully alert again, especially for older patients. Can everyone have general anaesthetic? Most people can have it safely, but in some cases, doctors may recommend alternatives. For example, if someone has severe heart or lung disease, regional anaesthesia (such as a spinal or epidural block) may be safer. Pregnant women, older people, and those with multiple medical problems require extra care, but general anaesthetic can still be given if needed. Are there long-term risks? For the vast majority, there are no long-term effects. Some people may feel tired for a few days or notice mild memory lapses, but these usually improve. Very rarely, complications such as nerve damage or awareness during surgery can occur, but these are exceptional. Research continues to study whether repeated anaesthesia has lasting effects, particularly in older people, but current evidence shows it is generally safe. How should
What is a Heart Bypass?
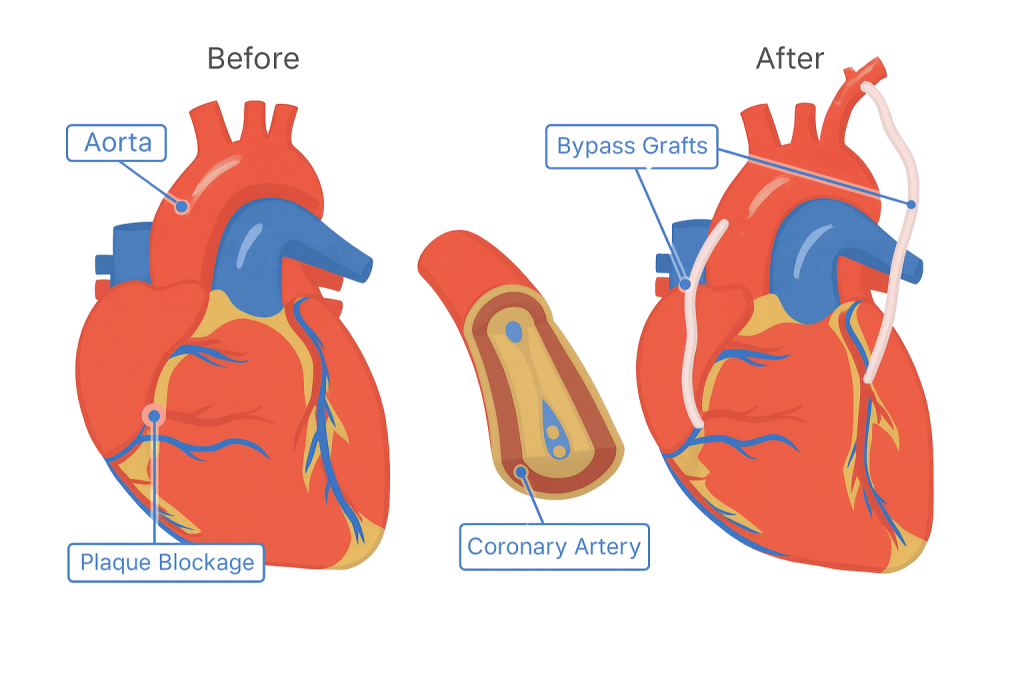
Seonat / August 22, 2025 / Cardiology What is a Heart Bypass? A heart bypass, is an operation that helps improve blood flow to the heart. It is usually carried out when the coronary arteries, which supply blood and oxygen to the heart muscle, have become blocked or narrowed. These blockages are caused by a build-up of fatty deposits called plaque, which reduce blood flow and can lead to chest pain, heart attacks, and other serious problems. During the operation, a surgeon takes a blood vessel from another part of your body often the leg, arm, or chest—and attaches it to the heart arteries, creating a new route for blood to flow. This new pathway “bypasses” the blockage, restoring good blood supply to the heart. Why would someone need a heart bypass? A heart bypass is usually recommended when a person has severe coronary heart disease and other treatments are not enough. For example, if medicines and lifestyle changes are not controlling chest pain, or if angioplasty (where a small balloon and stent are used to open an artery) is not suitable. People may also need a bypass if they have multiple blocked arteries, severe narrowing in the main artery of the heart, or if the heart muscle has already been damaged by a heart attack. Doctors weigh up the risks and benefits carefully before suggesting surgery. How does the operation work? The surgery is carried out under general anaesthetic, meaning the patient is asleep during the procedure. The surgeon takes a healthy blood vessel, known as a graft, from elsewhere in the body. The graft is then connected above and below the blockage in the coronary artery, creating a new route for blood. In many cases, the heart is temporarily stopped during the operation, and a heart-lung bypass machine takes over the job of circulating blood. In other cases, called “off-pump” surgery, the heart continues beating while the grafts are put in place. The approach depends on the patient’s health and the surgeon’s decision. How long does a heart bypass take? The length of the operation depends on how many arteries need to be bypassed. A single bypass might take three to four hours, while a more complex operation involving several arteries can take longer. After surgery, patients usually spend a short time in intensive care before moving to a hospital ward for further recovery. What is recovery like after a bypass? Recovery from a heart bypass takes time. Most people stay in hospital for around a week. At first, there may be some discomfort from the chest wound or the place where the graft was taken. Moving around feels difficult at first, but nurses and physiotherapists encourage gentle walking soon after the operation. Once home, full recovery can take several weeks to months. Patients are advised to avoid heavy lifting, gradually increase activity, and take part in a cardiac rehabilitation programme. These programmes include supervised exercise, education about diet and lifestyle, and support for emotional wellbeing. Is a heart bypass safe? Like any major surgery, a heart bypass carries risks. These include infection, bleeding, or reaction to the anaesthetic. Rarely, more serious complications such as stroke or heart attack can occur during or after the operation. However, for people with severe heart disease, the benefits of improving blood flow and reducing symptoms usually outweigh the risks. Advances in surgical techniques and aftercare mean the operation is safer today than ever before. How successful is a heart bypass? A heart bypass does not cure coronary heart disease, but it can greatly improve quality of life. Many people find their chest pain improves or disappears, and their risk of heart attack is reduced. The grafts usually last many years, though how long depends on lifestyle and other health conditions. Stopping smoking, eating a balanced diet, exercising, and taking prescribed medicines all help the grafts last longer. What is life like after a bypass? Most people return to normal activities after recovery, including work, hobbies, and exercise. Driving is usually possible again after six weeks, although this depends on the type of licence and personal recovery. Emotional recovery can take longer, as some people feel low or anxious after major surgery. Support from family, friends, and healthcare teams is important in this period. Are there alternatives to a heart bypass? In some cases, angioplasty and stents may be used instead of bypass surgery. This is less invasive and has a shorter recovery time, but it is not suitable for everyone. Medicines such as statins, beta-blockers, or nitrates may also help manage symptoms. The decision depends on the severity of the blockages, the number of arteries affected, and the overall health of the patient. How long do people live after a heart bypass? Many people live for years, or even decades, after bypass surgery. Survival depends on overall health, age, and lifestyle choices after the operation. Following medical advice and making healthy changes can extend life expectancy and reduce the risk of further problems. Regular check-ups with a doctor are important to monitor heart health and manage any ongoing conditions. Can healthy people ever need a bypass? Even people who appear healthy can sometimes need a heart bypass. This might be because of genetic factors, such as inherited high cholesterol, or because of silent heart disease that develops without clear symptoms. Routine health checks and paying attention to any new chest pain or breathlessness are key to spotting problems early. Does diet matter after a heart bypass? Yes, diet plays a big role in long-term recovery and preventing further problems. Doctors often recommend reducing saturated fats, eating more fruit, vegetables, and wholegrains, and cutting back on salt and sugar. These changes help lower blood pressure, cholesterol, and the risk of future blockages. Many hospitals include diet advice as part of cardiac rehabilitation. Summary Heart problems can show themselves in many ways, from chest discomfort and breathlessness to swelling, fatigue, or palpitations. Sometimes they are subtle and easy to dismiss, but knowing the
What is Menopause?
Seonat / August 21, 2025 / General Health What is Menopause? Menopause is when a woman stops having periods permanently. It happens because the ovaries stop releasing eggs and hormone levels such as oestrogen and progesterone drop. Doctors say a woman has reached menopause when she has not had a period for 12 months in a row. Menopause is something that every woman will experience in her lifetime, yet it can feel confusing or worrying if you do not know what to expect. It is a natural part of ageing, but because it can affect the body, mind, and daily life, many women want clear information about what it means. This guide explains menopause in simple terms, answers common questions, and looks at how it may be managed. For most women, this happens between the ages of 45 and 55, with the average in the UK being around 51. What are the symptoms? The symptoms of menopause can be different for everyone. Some women experience only a few, while others may notice many changes. Common symptoms include hot flushes, night sweats, changes in mood, poor sleep, vaginal dryness, reduced sex drive, and changes in memory or concentration. Some women also find their joints ache more or their hair and skin feel different. These symptoms happen because the body is adjusting to lower hormone levels. For some, they are mild and manageable. For others, they can be severe and affect daily life. What does perimenopause mean? Perimenopause is the stage before menopause. During this time, hormone levels start to change, and periods may become irregular. Some women start to notice hot flushes, mood swings, or heavier or lighter periods. Perimenopause can last several years, and it ends when periods stop completely. How long does menopause last? Menopause itself is a single point in time—the day 12 months after your last period. But symptoms linked to it can last for years. On average, women experience symptoms for around four to five years, though some may have them for a shorter or longer period. Is menopause the same for everyone? No, every woman’s experience is unique. Some women notice only mild symptoms, while others find their daily life is strongly affected. Family history can also play a role—if your mother experienced menopause earlier or later, you may too. Health conditions and lifestyle can also influence how symptoms feel and how long they last. How does menopause affect long-term health? Because oestrogen levels fall, menopause can increase the risk of certain health issues. These include osteoporosis (weaker bones), heart disease, and weight gain. It can also affect bladder health and dental health. This does not mean every woman will face these problems, but being aware of them can help with prevention through diet, exercise, and regular health checks. Can menopause affect mental health? Yes, many women notice changes in their mood. Some feel more anxious, irritable, or low in mood. This can be caused by hormone changes, poor sleep, or the stress of dealing with symptoms. Talking about these feelings and getting support from family, friends, or professionals can make a big difference. What treatments are available? There are several options to help manage symptoms. The most common is hormone replacement therapy (HRT), which replaces the hormones the body is no longer making. This can ease hot flushes, improve sleep, and protect against bone loss. Other treatments include lifestyle changes, such as regular exercise, healthy eating, stopping smoking, and reducing alcohol. Non-hormonal medicines and natural remedies are also sometimes used. The best treatment depends on each woman’s symptoms, age, and medical history. Should I go through the NHS or private care? In the UK, you can speak to your GP about menopause symptoms. They can offer advice, tests, and treatments such as HRT. For women who want faster appointments, more choice of treatments, or specialist care, private clinics are another option. The decision often depends on personal preference and budget. Can menopause be diagnosed with tests? Doctors usually diagnose menopause based on symptoms and age. Blood tests are sometimes used to measure hormone levels, especially for women under 45 or when the diagnosis is less clear. Most of the time, tests are not needed, as the symptoms and pattern of periods give enough information. What age is too early for menopause? Menopause before 40 is called premature menopause or premature ovarian insufficiency. It affects about 1 in 100 women. This can happen naturally or because of medical treatments such as surgery, chemotherapy, or radiotherapy. Women who experience menopause early may need extra support, including HRT, to protect bone and heart health. Can healthy women still struggle with menopause? Yes, even women with no health problems and active lifestyles can experience strong symptoms. Being healthy does not prevent menopause; it only helps manage its effects. For example, exercise and balanced eating may ease some symptoms, but they will not stop menopause from happening. Are there myths about menopause? Many myths surround menopause. Some people think it only affects older women or that symptoms are only about hot flushes. Others believe menopause means the end of sexuality or energy. These are not true. While menopause changes the body, many women find new ways to manage their health, relationships, and quality of life. What happens after menopause? Once menopause has passed, symptoms often lessen, although some may continue. The body adapts to lower hormone levels, and many women feel more stable again. However, the increased risks to bone and heart health remain, so staying active and having regular health checks is still important. Summary Menopause is a natural stage of life when periods stop, and hormone levels fall. It usually happens between ages 45 and 55, but symptoms and experiences vary widely. While some women notice only mild changes, others face difficult symptoms that affect daily life. Support is available through lifestyle changes, medical treatments such as HRT, and both NHS and private care. Understanding what is happening can make the journey easier and help women
What Are the Early Signs of Heart Problems?
Seonat / August 19, 2025 / Cardiology What Are the Early Signs of Heart Problems? Heart problems are a leading cause of illness and death in the UK, but spotting them early can make a big difference. Many people think heart disease only affects older men, but it can affect women, younger adults, and even people who seem healthy. Knowing the warning signs gives you a chance to act sooner and get checked before things become more serious. This guide looks at the common early signs of heart problems, why they happen, and what steps people often take afterwards. What do doctors mean by heart problems? The term “heart problems” covers a wide range of conditions that affect the heart’s structure or function. The most common is coronary heart disease, where fatty deposits build up in the arteries that supply blood to the heart. Other conditions include arrhythmias (irregular heart rhythms), heart valve problems, and heart failure, when the heart struggles to pump blood properly. While they all vary, many share similar early warning signs. Chest discomfort Chest pain or discomfort is one of the first things people associate with the heart. It might feel like pressure, tightness, heaviness, or burning. Sometimes it comes and goes, and sometimes it happens during exercise or stress. While not every chest pain is linked to the heart, chest discomfort should never be ignored. It can signal blocked arteries or reduced blood flow to the heart muscle. Shortness of breath Another early sign is feeling out of breath more easily than usual. This might happen during exercise, climbing stairs, or even when resting. Shortness of breath occurs because the heart is not pumping blood effectively, meaning less oxygen reaches the body. Some people also experience it when lying flat, which can be linked to early heart failure. Fatigue and weakness Feeling unusually tired or weak, even after resting, can sometimes point to heart problems. When the heart cannot pump enough blood around the body, muscles and tissues do not get the oxygen they need. People often dismiss this as stress or ageing, but unexplained fatigue is worth paying attention to, especially when it happens alongside other symptoms. Irregular heartbeat or palpitations The sensation that your heart is skipping beats, fluttering, or racing is called palpitations. While many cases are harmless, they can sometimes indicate arrhythmias. These irregular rhythms might not always cause noticeable symptoms, but when they do, they may leave you feeling dizzy, light-headed, or faint. Swelling in the legs, ankles, or feet The build-up of fluid in the lower body, called oedema, is another possible sign of heart trouble. It usually happens when the heart struggles to circulate blood properly, causing fluid to leak into surrounding tissues. Shoes feeling tighter or visible swelling at the end of the day can sometimes be linked to early stages of heart failure. Pain in other parts of the body Heart-related pain is not always felt in the chest. Some people notice pain spreading to the arms, neck, jaw, back, or stomach. Women, in particular, may experience heart symptoms in less typical ways, such as jaw pain, nausea, or back pain, rather than strong chest pain. Dizziness and fainting When the heart cannot maintain a steady rhythm or pump enough blood, blood pressure can suddenly drop. This can leave a person feeling dizzy, light-headed, or even cause fainting. While these symptoms have many possible causes, repeated episodes should be checked by a doctor. Nausea, sweating, or indigestion Some early heart problems can feel like indigestion, with nausea or stomach discomfort. Cold sweats or sudden clamminess can also occur during heart trouble, especially in cases of reduced blood flow. These symptoms are easy to mistake for other conditions, which is why they can often be missed. Are heart problems always obvious? Not always. Some people develop heart disease without experiencing any clear symptoms until the condition has progressed. Silent heart problems can sometimes be picked up during routine tests, such as blood pressure checks, cholesterol tests, or ECGs. This is why regular health checks are important, especially for people with risk factors like smoking, diabetes, or family history. How much does lifestyle affect early heart problems? Lifestyle plays a big role in heart health. Smoking, heavy drinking, poor diet, lack of exercise, and high stress can all increase the risk. On the other hand, regular exercise, eating balanced meals, and maintaining a healthy weight can lower the chance of developing symptoms. Even so, heart problems can still occur in people who appear healthy, which is why knowing the early signs is so important. Who is more at risk of developing heart problems? Heart problems are more common as people age, especially after 50. Men are slightly more likely to develop them earlier, although women’s risk increases sharply after menopause. People with high blood pressure, high cholesterol, obesity, or diabetes are also more prone to early symptoms. Family history plays a role too. For example, if a close relative developed heart disease at a younger age, your own risk may be higher. What tests can detect heart problems? Doctors use several tests to detect heart issues. These can include: Electrocardiogram (ECG): measures the heart’s electrical activity. Echocardiogram: uses ultrasound to look at the heart’s structure. Blood tests: check for signs of heart damage or high cholesterol. CT or MRI scans: provide detailed pictures of the heart and arteries. These tests help confirm whether symptoms are linked to heart disease or another condition. When should I see a doctor? If you notice any of the symptoms mentioned—especially chest pain, shortness of breath, or fainting—you should seek medical advice. For sudden or severe chest pain, you should call 999 immediately, as this could be a heart attack. For less urgent symptoms, booking an appointment with your GP is the best step or going to visit a private cardiology clinic like Heartsure. Can heart problems be treated if caught early? Yes. Treatments are much more effective when started early. This
Who is More Prone to Heart Disease?

Seonat / August 18, 2025 / Cardiology Who is More Prone to Heart Disease? Heart disease is a general term used to describe conditions that affect the heart and its blood vessels. The most common form in the UK is coronary heart disease, where the arteries supplying blood to the heart become narrowed or blocked. This can cause chest pain, heart attacks, and, in severe cases, heart failure. Other types of heart disease include arrhythmias (irregular heartbeats), congenital heart disease (problems you are born with), and valve disease, where the heart valves do not open and close properly. Heart disease remains one of the leading causes of illness and death in the UK, but the risks can be reduced with early detection and healthy lifestyle choices. Are There Specific Groups at Higher Risk? Yes, some groups of people are more prone to heart disease than others. Risk can increase due to age, gender, family history, and ethnicity. Men are generally at higher risk earlier in life, though women’s risk rises after the menopause. People from South Asian backgrounds have been shown to be more likely to develop heart disease at a younger age. Having close relatives with heart problems also increases your risk, particularly if they were diagnosed at a young age. Are There Specific Groups at Higher Risk? Yes, some groups of people are more prone to heart disease than others. Risk can increase due to age, gender, family history, and ethnicity. Men are generally at higher risk earlier in life, though women’s risk rises after the menopause. People from South Asian backgrounds have been shown to be more likely to develop heart disease at a younger age. Having close relatives with heart problems also increases your risk, particularly if they were diagnosed at a young age. Are There Different Types of Heart Disease? There are several types, each affecting the heart in different ways. Coronary artery disease is the most common, caused by a build-up of fatty deposits in the arteries. This is sometimes called atherosclerosis. Heart failure happens when the heart is too weak to pump blood properly. Arrhythmias are abnormal heart rhythms that can make the heart beat too fast, too slow, or irregularly. Valve disease affects the way blood flows through the heart, and congenital conditions are present from birth. Although these conditions are grouped together under “heart disease”, the risks and symptoms can vary depending on the type. What Tests Can Check for Heart Disease? If you are worried about heart disease, there are several tests your doctor might suggest. Blood tests can check cholesterol and blood sugar levels, which are linked to heart risk. An electrocardiogram (ECG) records the electrical activity of the heart and can spot irregular rhythms. An echocardiogram uses ultrasound to look at how the heart muscle and valves are working. CT coronary angiograms and MRI scans can give detailed pictures of the heart and arteries. In some cases, a treadmill stress test is used to see how the heart performs during exercise. Your GP will decide which tests are appropriate based on your symptoms, age, and risk factors. How Much Does Lifestyle Affect the Risk of Heart Disease? Lifestyle has a major impact on heart health. Diet, exercise, smoking, alcohol, and stress all play a role. Eating a diet high in salt, sugar, or saturated fat can raise blood pressure and cholesterol, which increases risk. Being physically inactive makes the heart less efficient and raises the chance of obesity, another risk factor. Regular exercise strengthens the heart and improves circulation. Stress can also contribute to unhealthy behaviours such as overeating, drinking more alcohol, or smoking. Together, these choices add up over time, making lifestyle one of the biggest influences on whether someone develops heart disease. Can Healthy People Get Heart Disease? Yes, even people who seem healthy can still develop heart disease. Some risk factors, such as family history, age, or certain medical conditions, cannot be controlled. For example, someone may eat well and exercise but still develop heart disease because of high cholesterol levels that run in their family. That is why regular health checks are important, even for people who feel well. What Age Group is Most at Risk? The risk of heart disease increases with age. In men, it often begins to rise after 45, while in women the risk rises after 55, particularly after the menopause. This is partly due to changes in hormone levels, which may provide some protection earlier in life. However, younger people are not immune. Poor lifestyle habits, obesity, and type 2 diabetes mean that more young adults are being diagnosed with heart problems today than in the past. How Bad is Smoking or Vaping for Heart Disease? Smoking is one of the biggest preventable causes of heart disease. It damages the lining of the arteries, makes blood more likely to clot, and reduces oxygen in the blood. All of these changes put extra strain on the heart. Smokers are much more likely to have a heart attack than non-smokers. Vaping is newer, and research is still ongoing. Early studies suggest that vaping may also affect blood vessels and raise the risk of heart problems, though likely less than smoking. However, because it often contains nicotine, it can still increase blood pressure and heart rate. Most experts agree that the safest choice for heart health is to avoid both smoking and vaping. Do Studies Show Links Between Traits and Heart Disease? Yes, many large studies have looked at the traits linked with heart disease. High blood pressure, high cholesterol, and diabetes are the strongest risk factors. Being overweight, especially carrying extra fat around the waist, is also linked with greater risk. Genetics play a role, as people with a family history are more likely to develop it themselves. Research has also shown that people from certain ethnic backgrounds, particularly South Asian and African-Caribbean communities, are more likely to develop heart disease at younger ages and sometimes more severely. UK Biobank
What is an Echocardiogram?
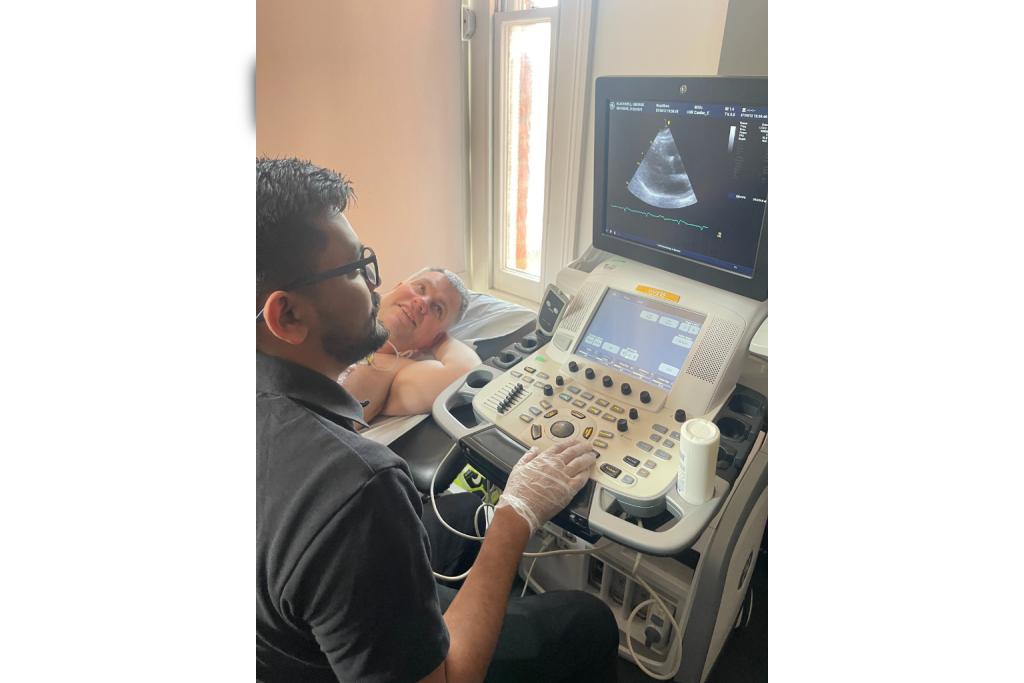
Seonat / August 17, 2025 / Cardiology What is an Echocardiogram? An echocardiogram, often called an “echo”, is a heart scan. It uses sound waves, known as ultrasound, to create moving pictures of the heart. Unlike X-rays or CT scans, an echocardiogram does not use radiation. Instead, it works in the same way as the scans used during pregnancy. Doctors use echocardiograms to see how the heart muscle, valves, and blood flow are working. It is one of the most common heart tests in the UK and is widely used in both hospitals and specialist heart clinics. What Does an Echocardiogram Show? The images from an echocardiogram can show a lot of detail about the heart’s structure and function. Doctors can see the size of the heart and whether it is pumping strongly enough. They can check if the valves are working properly or if blood is leaking through them. The scan can also show blood clots, fluid around the heart, or signs of infection and damage after a heart attack. By giving a clear picture of how the heart is working in real time, an echocardiogram helps doctors diagnose problems such as heart failure, valve disease, or congenital heart conditions that may be present from birth. It can also be used to track how these conditions change over time. Actual results of an Echocardiogram scan of a female. How Does it Work? An echocardiogram works by using ultrasound technology. A small device called a transducer is placed on the chest and gives out high-frequency sound waves. These sound waves bounce off the structures of the heart, and the returning echoes are picked up by the transducer. A computer then turns them into moving images. On the screen, doctors can see the heart beating and blood moving through it. Some machines add colour to show the direction of blood flow, which makes it easier to see if blood is going the wrong way or if a valve is not closing properly. What to Expect During the Test The test is usually done while you are lying on a bed in a hospital department or clinic. A healthcare professional will put a small amount of gel on your chest, which helps the sound waves travel. The transducer is then moved across the chest to capture images from different angles. Sometimes you may be asked to roll onto your side or hold your breath for a few seconds to make the pictures clearer. The test is painless, though pressing the transducer firmly on the chest may feel a little uncomfortable. You may also notice the gel feels cool when it is applied. The whole process usually takes between 20 and 40 minutes, and you can go home straight afterwards. Simple carousel diagram to show the Echocardiogram procedure. Different Types of Echocardiogram The most common type is called a transthoracic echocardiogram, where the transducer is placed on the chest. In some cases, doctors may need a clearer picture of certain areas, so they use a transoesophageal echocardiogram. For this test, the transducer is placed on a thin tube and gently guided down the throat into the oesophagus, which sits close to the heart. This gives sharper images, but it is slightly more invasive and often done under light sedation. Another type is a stress echocardiogram. This test looks at how the heart works when it is beating faster, either after exercise or after being given medicine that increases heart rate. Echocardiograms can also be done during pregnancy to check a baby’s heart, known as a foetal echocardiogram. Is it Safe? Echocardiograms are very safe. Because they use sound waves instead of radiation, they can be performed on adults, children, and even unborn babies without risk. The standard test is non-invasive and has no side effects. The more specialised transoesophageal echocardiogram carries a small risk, as it involves passing a probe down the throat, but it is generally very safe when carried out by trained staff. Any mild risks are far outweighed by the benefits of having clear information about the health of your heart. Who Performs an Echocardiogram? The test is usually carried out by a sonographer, who is a healthcare professional trained in ultrasound scanning, or by a cardiologist, who is a doctor specialising in the heart. They record the images during the test, and then a cardiologist interprets the results. The cardiologist looks for problems with the heart muscle, valves, or blood flow and decides whether treatment or further tests are needed. What Happens After the Test? Most people can leave straight after a standard echocardiogram. If you had a transoesophageal echo, you may need to wait until the sedation has worn off before going home. The results are not usually given immediately, as they need to be carefully reviewed. A cardiologist will analyse the images and write a report, which is sent to your GP or specialist. They will then explain what the results mean and discuss the next steps, if any. Common Questions About Echocardiograms One of the most common questions people ask is whether the test hurts. The answer is no. At most, you might feel mild pressure from the transducer on your chest, but the scan itself is painless. Another question is whether you can eat or drink before the test. For a standard echo, there are no restrictions, but for a transoesophageal echo you will usually be asked not to eat for a few hours beforehand. Many people also wonder how long they will need to stay in hospital. For the majority of tests, you can go home straight away, unless sedation was used. Parents often ask if children can have echocardiograms, and the answer is yes. The test is safe for children and even for newborn babies. Results are usually available within a few days, although urgent cases may be reported more quickly. How Often Should I Have an Echocardiogram? Echocardiograms are widely available on the NHS if your doctor thinks you need one,
What is a CT Coronary Angiogram?
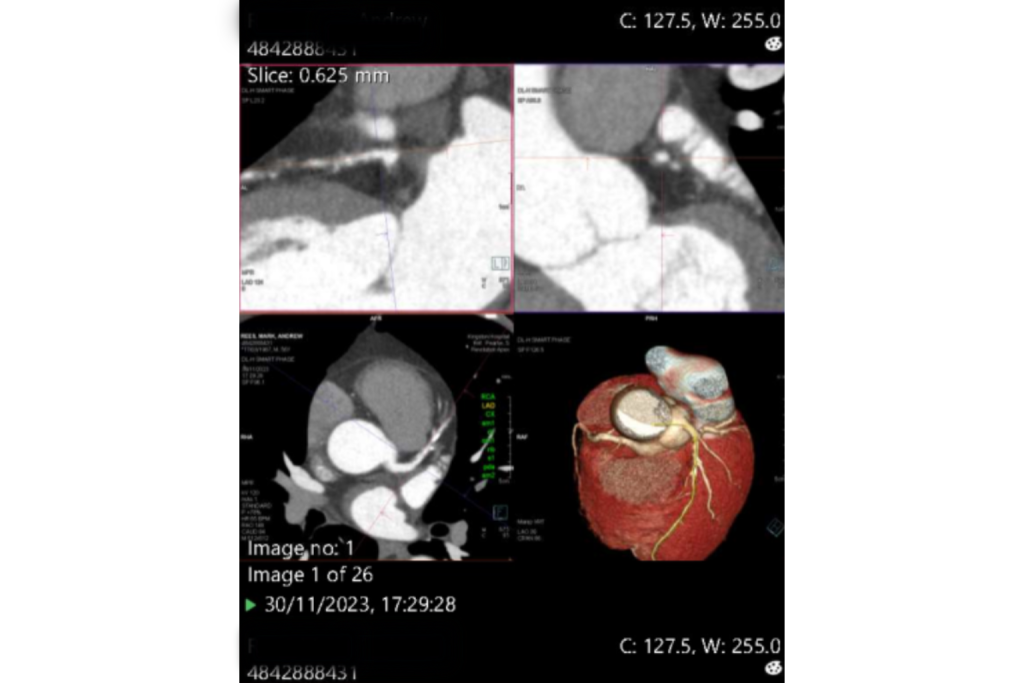
Seonat / August 15, 2025 / Cardiology What is a CT Coronary Angiogram? A CT coronary angiogram is a special type of heart scan. It uses a CT scanner to take detailed pictures of your heart and its blood vessels. Simple carousel diagram to show the CT coronary angiogram procedure. The pictures are taken after a dye called contrast is injected into your bloodstream, which makes the arteries show up clearly. Doctors use this test to check for problems with the heart’s blood vessels, called the coronary arteries. These arteries carry blood to the heart muscle. If they become narrowed or blocked, it can lead to chest pain or increase the risk of a heart attack. What Do They Detect or Show? A CT coronary angiogram can show if your coronary arteries are narrowed, blocked, or have a build-up of fatty deposits called plaque. It can also reveal other heart problems, such as unusual artery shapes or signs of injury. The images give doctors a clear view of how blood is flowing to your heart. This information helps them decide if treatment is needed, such as lifestyle changes, medication, or further procedures. Actual results of a CTCA scan for a male. Can They Be Used to Check for Heart Disease? Yes. A CT coronary angiogram is often used to check for signs of coronary artery disease. This is when the arteries supplying blood to the heart become narrowed due to plaque build-up. By showing how open or blocked the arteries are, the scan can help doctors decide whether you might benefit from treatments like medicines to lower cholesterol or, in more severe cases, surgery or stents to improve blood flow. How Does it Work? The scan is done in a hospital radiology department. First, you are given an injection of contrast dye, usually into a vein in your arm. The dye travels through your bloodstream and makes the coronary arteries show clearly on the scan. You will lie on a table that moves slowly through the CT scanner, which is shaped like a large ring. The scanner uses X-rays to take detailed cross-section images of your heart and blood vessels from different angles. A computer then combines these into a full 3D picture. Sometimes, you may be given medicine before the scan to slow your heart rate. This helps the images come out clearer. Is it Safe? For most people, a CT coronary angiogram is safe. The scan does involve a small amount of radiation, similar to other CT scans, but the benefits of detecting heart problems often outweigh the risks. The contrast dye is safe for most people but can rarely cause allergic reactions. People with kidney problems may need extra checks before having the dye. Pregnant women are usually advised to avoid this scan unless it is urgently needed. Common Questions About CT Coronary Angiograms Does it hurt?No, the scan is painless. You may feel a cool sensation when the dye is injected, and the table might feel a little firm, but the process is comfortable for most people. Do I need to stay in hospital afterwards?No, you can usually go home the same day. If you’ve had medication to slow your heart rate, you might need to rest for a short time before leaving. How long does it take?The scan itself takes only a few minutes, but you may be in the department for 30–60 minutes to prepare and have your heart rate checked. What Happens After the Scan? Once the scan is complete, a radiologist — a doctor who specialises in medical images — will look at the pictures and write a report. The report is sent to your cardiologist or the doctor who referred you. Your doctor will discuss the results with you. If narrowing or blockages are found, they will explain your treatment options. This could include lifestyle advice, medicines, or further tests such as an invasive coronary angiogram. Private Cost Comparison CT Coronary Angiogram vs Invasive Angiography Price difference between a CTCA scan and an invasive Angiogram scan. Sources: Heartsure, KIM’s Hospital Should I Go Through the NHS or Private? In the UK, CT coronary angiograms are available on the NHS if your doctor thinks you need one. The NHS covers the cost, but waiting times can vary depending on your local hospital and how urgent your case is. Private healthcare can sometimes offer quicker appointments and more flexibility in choosing when and where you have the scan, but you will need to pay for it or use private medical insurance. Average NHS Wait Time for CT Coronary Angiogram Average wait times for patients to have an CTCA scan in the UK (NHS vs. Private) Sources: NHS How Often Should I Get a CT Coronary Angiogram? Most people do not need this scan regularly. It is usually done when there is a medical reason, such as chest pain, abnormal heart test results, or a high risk of coronary artery disease. Your doctor will decide if and when you need one based on your symptoms and health history. Routine scanning without symptoms is not generally recommended because it involves radiation and contrast dye, and the benefits are small if you have no signs of heart disease. Factors That Might Mean You Need One You may be referred for a CT coronary angiogram if: You have chest pain that could be related to heart problems. Other tests, like an ECG or exercise test, show changes that suggest heart disease. You have a strong family history of early heart problems. You have high risk factors, such as high blood pressure, diabetes, high cholesterol, or smoking. Your doctor will weigh your personal risk and decide if the scan is the best next step. Are There Alternatives to a CT Coronary Angiogram? Yes. In some cases, other tests can provide similar information. These include: Invasive coronary angiogram — where a thin tube is inserted into the blood vessels and dye is injected directly into the heart arteries.
What is a Radiologist?

Seonat / August 14, 2025 / Radiology What is a Radiologist? A radiologist is a doctor who looks at pictures of the inside of your body, such as X-rays, MRI scans, and CT scans, to help find out what might be wrong. Radiologists don’t usually meet patients for long appointments like GPs do. Instead, they work behind the scenes, carefully studying images and writing reports for the doctors who referred the patient for the scan. Their work is important because many health conditions can only be confirmed with imaging. What Do They Actually Do? A radiologist’s main job is to interpret, or “read”, the images taken during medical tests. They use their knowledge of anatomy, disease, and imaging technology to spot signs of illness, injury, or changes in the body. Some radiologists also carry out image-guided procedures. This can include guiding a needle for a biopsy, draining fluid from an organ, or helping with certain treatments such as targeted cancer therapies. How Do You Become a Radiologist? In the UK, becoming a radiologist takes many years of study and training. First, they must complete a medical degree, which usually takes five or six years. After this, they work as a junior doctor in hospitals, gaining experience in different areas of medicine. Then they apply for specialist radiology training, which lasts at least five years. During this time, they learn how to use different imaging technologies, how to spot different diseases, and how to perform image-guided treatments. Many radiologists also train in a sub-specialty, such as paediatric radiology (for children) or neuroradiology (for the brain and nervous system). What Types of Radiologists Are There? There are several types of radiologists, each focusing on different areas of the body or types of imaging: Diagnostic radiologists – interpret images to help diagnose illnesses or injuries. Interventional radiologists – use imaging to guide small procedures or treatments. Oncological radiologists – focus on diagnosing and sometimes helping treat cancers. Paediatric radiologists – specialise in imaging for children and babies. Each type of radiologist plays a key role in helping other doctors make the best decisions for patient care. Where Do Radiologists Work? Radiologists work in hospitals, private clinics, and specialist imaging centres. In large hospitals, they may be part of a big imaging department, working alongside radiographers (who operate the machines) and other healthcare staff. Some radiologists work for the NHS, others in private healthcare, and some do both. In many cases, their work is done in quiet reporting rooms where they can focus on studying the images without distractions. How Does a Radiologist Fit Into My Care? If your GP or hospital doctor sends you for an imaging test, the scan or X-ray will be carried out by a radiographer or another imaging specialist. Once the pictures are taken, they are sent to the radiologist. The radiologist will carefully examine the images, sometimes comparing them to older scans to see if there have been changes. They will then write a detailed report explaining what they found. This report goes back to your doctor, who will use it to plan your treatment or decide if more tests are needed. Technology Used in Radiology Radiology relies on a range of imaging technologies, including: X-ray – For bones, chest, and certain other body areas. CT scans – For cross-sectional images of the body. MRI scans – For detailed pictures of soft tissues. Ultrasound – For pregnancy scans, organ checks, and blood flow assessment. In recent years, artificial intelligence (AI) has started to support radiologists by identifying patterns in images and flagging areas that might need closer examination. AI can speed up analysis, but the radiologist always makes the final judgement. Different radiology machines How Long Does it Take for a Radiologist to Report Results? The time it takes for a radiologist to report on a scan depends on the urgency of the case. In emergencies, such as a suspected stroke or internal bleeding, the report can be done in minutes so treatment can start immediately. For routine scans, it may take a few days for the report to be completed and sent to your doctor. Delays can happen if the hospital is very busy, but urgent cases are always prioritised. Common Questions About Radiologists Do radiologists perform surgery?Interventional radiologists sometimes perform small, minimally invasive procedures, but they do not carry out large operations like surgeons. Is a radiologist the same as a radiographer?No. A radiographer operates the scanning equipment, while a radiologist is a doctor who interprets the images. Can radiologists work remotely?Yes. Many radiologists can report on scans from different locations using secure computer systems, which is known as teleradiology. Do radiologists only work with humans?Most radiologists work in human medicine, but there are also veterinary radiologists who work with animals. RCR Radiologist Workforce Figures Royal College of Radiologists (RCR) data for consultant clinical radiologists in the UK Sources: RCR Clinical Radiology Census Report 2019, Census Report 2021, Clinical Radiology Workforce Census 2023 The Future of Radiology Radiology is evolving quickly. Developments include: More advanced scanners that produce clearer images in less time. AI assistance to speed up image review. Better interventional techniques that treat problems without major surgery. As technology progresses, radiologists are expected to take on even more complex diagnostic and treatment roles. A Simple Summary A radiologist is a highly trained doctor who specialises in reading medical images. They work closely with other healthcare professionals to diagnose and help treat a wide range of conditions. While you might not always meet them, their role is essential in modern medicine. They interpret scans such as X-rays, CT scans, MRI scans, and ultrasounds, and their reports guide your doctor in making the right decisions for your care. Disclaimer: Seonat provides general health information for educational purposes only. This content is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your GP or another qualified health provider with any questions about a medical condition or before making health decisions.
